Journal Digest
Buprenorphine Outperforms Morphine for Neonatal Abstinence Syndrome

Buprenorphine is a more effective treatment for neonatal abstinence syndrome (NAS) than the current standard of morphine, reports a study published in the New England Journal of Medicine.
The study involved 63 full-term infants who had been exposed to opioids in utero and had signs of NAS, including irritability, tremor, and poor feeding. The infants were randomized to receive either sublingual buprenorphine (0.075 mg/ml every 8 hours) or oral morphine (0.4 mg/ml every 4 hours) until they stopped showing symptoms of NAS. Infants with symptoms that were not controlled by the assigned opioid were treated with adjunctive phenobarbital.
Compared with morphine, the group receiving buprenorphine had on average shorter treatment durations (15 days versus 28 days) and shorter hospital stays (21 days versus 33 days). There was no significant difference between the number of infants in both groups that required adjunctive phenobarbital (five in the buprenorphine group versus seven in the morphine group).
Rates of adverse effects were also similar between the two groups. However, the study authors noted that buprenorphine did not lower the respiratory rate as much as morphine did. “This potential advantage, along with a longer interval between doses, may allow for investigation of buprenorphine in outpatient settings,” the authors wrote.
Kraft W, Adeniyi-Jones S, Chervoneva I, et al. Buprenorphine for the Treatment of the Neonatal Abstinence Syndrome. N Engl J Med. May 4, 2017. [Epub ahead of print]
Mobile Version of CBT-I Found to Be Effective

Cognitive-behavioral therapy for insomnia (CBT-I) has shown effectiveness in both face-to-face and online formats. A study in the Journal of Medical Internet Research now reports the first randomized trial of a mobile phone version of CBT-I.
A total of 151 adults with a history of mild insomnia were assigned to receive either the mobile CBT-I application for six to seven weeks or be placed on a wait list. The app, known as Sleepcare, packages together a sleep diary, relaxation exercises, and educational materials about sleep and sleep hygiene.
At the conclusion of the study, the investigators found that the group receiving the app showed significant improvements in both insomnia severity and sleep efficiency, and these improvements were retained at a three-month follow-up visit. In general, the size of the improvements was about the same as observed for other web-based CBT-I approaches.
Horsch C, Lancee J, Griffioen-Both F, et al. Mobile Phone-Delivered Cognitive Behavioral Therapy for Insomnia: A Randomized Waitlist Controlled Trial. J Med Internet Res. Apr 11, 2017; 19(4): e70.
Baclofen Incites Earlier Reaction to Alcohol
Baclofen—a GABA receptor agonist—has been studied as a potential medication for alcohol use disorder. A small study in Translational Psychiatry found that while patients administered the medication did not drink less, they did report a greater response to alcohol.
The study enrolled 34 anxious, alcohol-dependent individuals and randomized them to receive either 30 mg baclofen or placebo for at least eight days. Each participant then took part in a monitored alcohol self-administration test to assess desire to drink.
There were no differences in average alcohol consumed between baclofen and placebo, with both groups drinking around 43 to 45 grams. However, the baclofen group reported higher intoxication feelings after taking their initial “priming” drink, and they also reported greater ratings of feeling high or intoxicated during the test. In addition, heart rate was greatly reduced in the baclofen group.
“Hypothetically, amplification of subjective responses to alcohol after an initial drink may reduce the amount of subsequent alcohol drinking as the desired effects have already been achieved,” the authors wrote.
Farokhnia M, Schwandt M, Lee M, et al. Biobehavioral Effects of Baclofen in Anxious Alcohol-Dependent Individuals: A Randomized, Double-Blind, Placebo-Controlled, Laboratory Study. Transl Psychiatry. Apr 25, 2017; 7(4):e1108.
Amitriptyline May Improve Blood-Brain Barrier Permeability
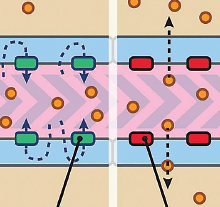
The tricyclic antidepressant amitriptyline may make it easier for drugs to pass through the blood-brain barrier, according to a study in the Journal of Cerebral Blood Flow and Metabolism.
For the study, researchers at the National Institute of Environmental Health Sciences started by treating isolated capillaries from rats with lysophosphatidic acid (LPA). LPA reduced the activity of P-glycoprotein, a cellular protein found on the brain’s border that actively pumps drugs and other chemicals back into the bloodstream.
They next administered amitriptyline (this drug also interacts with LPA-related signaling pathways) to the capillaries and found that it could also rapidly turn off P-glycoprotein activity. This inhibition was reversible, as P-glycoprotein pump activity returned to normal once the amitriptyline infusions stopped.
These experiments were successfully conducted in blood vessels from both normal rats and a rat model of amyotrophic lateral sclerosis (ALS).
“Activating an endogenous phospholipid-induced signaling cascade at the capillary endothelium with nanomolar concentrations of a therapeutic already present in the clinic may provide a safe and effective means to target P-glycoprotein while avoiding side effects associated with dosing and specificity,” the authors wrote.
Banks D, Chan G, Evans R, et al. Lysophosphatidic Acid and Amitriptyline Signal Through LPA1R to Reduce P-glycoprotein Transport at the Blood-Brain Barrier. J Cereb Blood Flow Metab. April 27, 2017. [Epub ahead of print]
People With Mental Illness May Seek More Acute Care Following Bariatric Surgery
An assessment of health records from 8,192 patients who had undergone bariatric surgery found that preoperative mental illness was not associated with less postoperative weight loss.
However, patients with severe depression or anxiety disorder, bipolar disorder, or schizophrenia did have more follow-up emergency department (ED) visits and longer hospital stays compared with patients with no mental illness.
One year after surgery, for example, patients with severe depression or anxiety (n=500) were about 30 percent less likely to have zero ED visits and 60 percent less likely to have zero hospital stays compared with surgery patients with no preoperative mental illness.
Patients with bipolar disorder, schizophrenia, or psychosis (n=508) were 40 percent less likely to have zero ED visits and 50 percent less likely to have zero hospital stays. These risks persisted two years after the surgery.
“This finding underscores the need to explore tailored, supportive postoperative outreach to minimize the risk of adverse health outcomes among patients with known mental illness,” the study authors wrote.
The records were from bariatric patients across seven health care systems in the United States that are part of the Patient Outcomes Research to Advance Learning (PORTAL) network. This analysis was published in the journal Obesity. ■
Fisher D, Coleman K, Arterburn D, et al. Mental Illness in Bariatric Surgery: A Cohort Study From the PORTAL Network. Obesity. May 2017; 25(5): 850-856.



