Opioid Prescribing Falls But Still Remains High
Abstract
Several states that have been hit hardest by the opioid epidemic have taken strides—such as mandated use of Prescription Drug Monitoring Programs—that have proven successful.
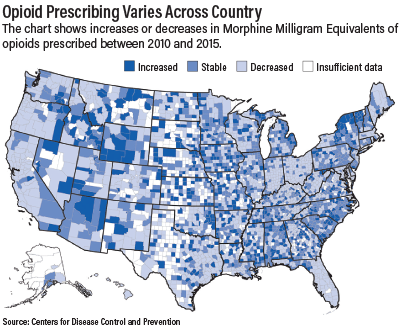
Opioid prescribing decreased in parts of the country between 2010 and 2015, but remains high compared with 1999 levels, according to a report by the Centers for Disease Control and Prevention (CDC).
The amount of opioids prescribed in the United States peaked at 782 morphine milligram equivalents (MME) per capita in 2010 and then decreased to 640 MME per capita in 2015, the CDC reported in the July 7 Morbidity and Mortality Weekly Report (MMWR).
Addiction experts say the finding is a ray of hope in the midst of the nation’s opioid overdose epidemic. Yet despite the significant decreases, the amount of opioids prescribed per person in 2015 remained approximately three times as high as in 1999 and varied substantially across the country. County-level factors associated with higher amounts of prescribed opioids include a larger percentage of non-Hispanic whites, a higher prevalence of diabetes and arthritis, and higher unemployment and Medicaid enrollment, according to the CDC.
Moreover, opioid-involved overdose death rates continue to increase, though the CDC noted that these increases have been driven largely by use of illicit fentanyl and heroin. “There is no evidence that policies designed to reduce inappropriate opioid prescribing are leading to these increases,” the MMWR report stated.
The CDC analyzed retail prescription data from QuintilesIMS to assess opioid prescribing in the United States from 2006 to 2015, including the rates, amounts, dosages, and durations. County-level prescribing patterns in 2010 and 2015 were also analyzed.
The CDC found that in the United States, annual opioid prescribing rates increased from 72.4 to 81.2 prescriptions per 100 people from 2006 to 2010, were constant from 2010 to 2012, and then decreased by 13.1 percent to 70.6 per 100 people from 2012 to 2015. Annual high-dose opioid prescribing rates remained stable from 2006 to 2010 and then declined by 41.4 percent from 11.4 per 100 people in 2010 to 6.7 in 2015.
Several states that have been especially hard hit by the epidemic—Florida, Kentucky, and Ohio—have taken forceful measures to reduce prescribing that have shown impressive results. “In 2011 and 2012, Ohio and Kentucky, respectively, mandated that clinicians review Prescription Drug Monitoring Program (PDMP) data and implemented pain clinic regulation,” the report stated. “MME per capita decreased in 85 percent of Ohio counties and 62 percent of Kentucky counties from 2010 to 2015. In Florida, where multiple interventions targeted excessive opioid prescribing from 2010 through 2012 (such as pain clinic regulation and mandated PDMP reporting of dispensed prescriptions), the amount of opioids prescribed per capita decreased in 80 percent of counties from 2010 to 2015. Florida also experienced reductions in prescription opioid-related overdose deaths.”
John Renner, M.D., vice chair of APA’s Council on Addiction Psychiatry, said the CDC results are a positive sign. “It’s clear that various agencies of the government and concerned national groups have come forward with a strong and consistent message that more conservative prescribing of opioids is necessary,” Renner told Psychiatric News. “The CDC report suggests that physicians are getting the message—not everyone is, but many are. Certainly, the Prescription Drug Monitoring Programs are important, and the states that make use of them are getting better outcomes.”
Nonetheless, Renner cautioned against what he called a “ham-fisted” approach to the problem whereby some physicians may too abruptly curtail opioid prescribing for patients. “If you push too far in the opposite direction, you run the risk of making the problem worse,” he said. “I am hearing anecdotally about patients who are dropped from treatment or abruptly tapered off who then go out seeking pills.”
Renner also said that more and better public education about pain and pain management is needed to counter the effects of pharmaceutical advertising directed at consumers. “Physicians don’t practice in a vacuum,” he said. “Patients are bombarded by advertisements and the meta-message is that there are meds out there that should make you feel good, with a quick fix.”
Psychiatrist Patrice Harris, M.D., who is the immediate past chair of the American Medical Association Board of Trustees and chair of the AMA Task Force to Reduce Opioid Abuse, agreed the CDC results indicate progress is being made.
“The AMA is pleased that national prescribing data confirm that for the past several years physicians have made more judicious prescribing decisions, but continued progress and improvements are necessary,” she said in a statement.
“The Centers for Disease Control and Prevention’s report also reinforces two critical elements that must be addressed if the nation’s opioid epidemic is to be reversed. First, our country must do more to provide evidence-based, comprehensive treatment for pain and for substance use disorders. This can be accomplished, in part, by implementing the National Pain Strategy and reducing barriers to all modalities for treating pain. ... Second, physicians must continue to lead efforts to reverse the epidemic by using prescription drug monitoring programs, eliminating stigma, prescribing the overdose-reversal drug naloxone, and enhancing their education about safe opioid prescribing and effective pain management.” ■
“Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015” can be accessed here.



