Survey Finds EHRs Contribute to Burnout
Abstract
Documenting extensive patient details and creating alerts for other physicians may be a sound strategy for good patient care, but the increased time spent on health records can take a toll on physicians and patients.
Most research efforts on physician burnout have focused on traditional risk factors that may lead to emotional exhaustion, depersonalization (feeling cynical or detached from patients), and decreased sense of accomplishment. These factors include long work hours, financial strain, and difficult mentor relationships. One risk factor that has been identified more recently is the electronic health record (EHR).

Though EHRs have centralized patient information, their importance in many health care systems is leading physicians to spend more time facing a computer screen in lieu of facing their patients. The field of psychiatry, in particular, can be prone to EHR overuse, according to Nicholas Domaney, M.D., a clinical fellow of psychiatry at Harvard’s Beth Israel Deaconess Medical Center.
“Psychiatry notes can get quite lengthy at times,” he said. “They usually include lots of details about a patient’s history and the family history, for example.”
Another issue with EHR systems is the growing prevalence of pop-up alerts that notify physicians about changes in patient status or potential risks with prescribed medications. Pop-up alerts were initially developed as a way to reduce physician error, but their overabundance has led physicians to ignore a large majority of them. Some studies have also shown that these alerts are a contributor to EHR-related burnout.
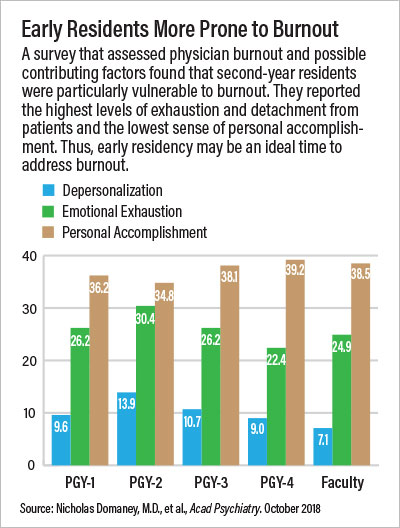
Discussions with colleagues about the burden of EHRs led Domaney and fellow Harvard psychiatrists John Torous, M.D., and William Greenberg, M.D., to conduct a survey of their department’s residents and faculty about EHR use. Though the sample size was modest (40 residents and 12 faculty), the survey did reveal a clear correlation between time spent on EHRs and burnout symptoms, particularly emotional exhaustion and a lack of personal accomplishment.
Second-year residents reported the highest rates of symptoms in each of the three classic domains of burnout—emotional exhaustion, depersonalization, and lack of personal accomplishment. “In our program, this is the time where residents spend the largest amount of time on call,” Domaney said.
While that extended time in emergency departments and consultation sessions creates a lot of stress and fatigue, it also involves more documentation.
“Little time is built into physicians’ schedules to handle all this work,” said Hardeep Singh, M.D., M.P.H., a research scientist at the Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VA Medical Center in Houston and a professor of medicine at Baylor College of Medicine. “Doctors have to carve out time at the end of the day or on weekends. That can impact their well-being, especially if there are administrative demands to close a patient’s chart within a certain time.”
In addition, incorrect data from a hastily written EHR note or unread alert pose safety risks to patients, Singh said.
Domaney added that the connection between time spent on EHRs and burnout in residents does not imply that EHRs are solely driving stress and burnout; more likely on-call fatigue, excess EHR use, and other burnout risk factors all interact and reinforce each other.
“One of the most notable findings from the survey, though, was that the negative effects of EHR use were slightly stronger than the positive emotional effects of sleep, exercise, and participating in outside activities,” Domaney said. “Most anti-burnout programs are focused on wellness; that is definitely important, but the survey suggests wellness alone is not enough.”
Singh, who has also published research linking EHR workload to burnout, told Psychiatric News that modifying how EHRs are used will require health care professionals at all levels to play a role. At an administrative level, hospital leaders could receive weekly summaries of alerts that might detail who has received the most or who has ignored the most.
“These data might help administrators identify doctors at more risk of the negative consequences of EHRs,” he said. Singh also believes that EHR systems need to be made more customizable, even though that may make it difficult for various hospital departments to communicate.
However, there are some steps that health care professionals can take to lessen the administrative burden of EHRs. One of the simplest is to learn how to type efficiently—it can save time and frustration. Another option is to consider limiting the people who receive EHR-related alerts when updating a record.
“We have developed into a bit of an FYI culture where we feel everyone needs to know what’s going to happen next,” he said. “But every alert adds more work not just for you but everyone who reads it.”
Domaney agreed that a more streamlined approach to EHR documentation is needed. “There has been a perception that if we enter more information into the record, we are providing better care,” said Domaney. “But maybe if we take a step back and look at how and why we document certain items, we can find a way to be more efficient about our entries.” ■
“Exploring the Association Between Electronic Health Record Use and Burnout Among Psychiatry Residents and Faculty: A Pilot Survey Study” can be accessed here.



