Researchers Sum Up Current Knowledge of Bipolar Disorder, Call for More Study
Abstract
Researchers confirm the progressive nature of bipolar disorder and find early intervention may prevent the more disabling aspects of the disorder.
The progressive nature of bipolar disorder, with milder phases occurring prior to the classic onset of the disease, makes it an ideal candidate for early intervention strategies, according to a research review published January 24 in AJP in Advance.
Bipolar disorder affects 1 percent of the world’s population, and it is more prevalent in this country than in Canada and Europe, according to Eduard Vieta, M.D., Ph.D., of the Barcelona Bipolar Disorders Program at the University of Barcelona and colleagues. Mood symptoms emerge for up to 70 percent of individuals with the disorder before age 21.
For the review, the researchers examined more than 50 original studies evaluating prodromal symptoms and risk factors; biomarkers; screening tools; and early intervention treatment options, including psychotherapeutic and pharmacological interventions, for bipolar disorder.
Early identification may prevent or at least delay the onset of the disorder, co-author Boris Birmaher, M.D., the endowed chair in Early Onset Bipolar Disease and a professor of psychiatry at the University of Pittsburgh School of Medicine, told Psychiatric News. “This can give the young person a chance to develop normally, to finish school or maybe go to college, to foster interpersonal relationships, and to develop good coping skills before the full illness strikes.”
Failing to recognize and treat patients in the earliest stages of the disorder carries a high cost, such as increased risk for dropping out of school, using drugs, or death by suicide, Birmaher added. “The longer you wait, the more resistant to treatment this illness is.”
A move toward early intervention will require changes in health insurance and government policies that dictate access to care, as well as better education of mental health professionals, general practitioners, and even the general public, co-author Estela Salagre, M.D., the scientific director assistant in the research consortium CIBERSAM (Centro de Investigación en Red de Salud Mental) and researcher in the Bipolar Disorders Unit of the Clinical Institute of Neuroscience in Barcelona, told Psychiatric News. “Social stigma, too, is one of the biggest barriers to early intervention.”
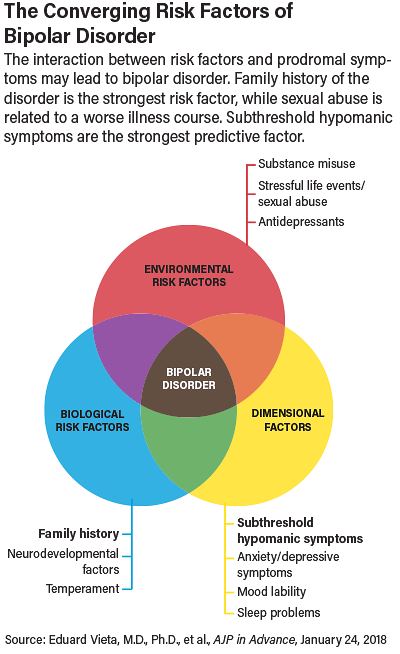
Bipolar disorder has a high genetic loading: the single greatest risk factor for developing the disorder is having a parent with the illness, particularly one who had an onset of the disease before age 21, the authors concluded. However, such children are also at increased risk for other psychopathology, such as major depressive disorder, anxiety disorder, or attention-deficit/hyperactivity disorder (ADHD), rendering a correct diagnosis more challenging.
Among the prodromal symptoms, the strongest predictor of conversion to bipolar disorder is subsyndromal manic symptoms, the authors wrote. Young people with these symptoms tend to have recurrent episodes of hyperactive, silly, and disruptive behaviors at school and home, beyond what are expected for their age, Birmaher said. For example, patients’ parents comment that they cannot take their child to church. Unlike children with ADHD, the problems of these children are not continuous; they may last a few months and then stop, only to emerge again later. Sometimes a child becomes grandiose—for instance, he may genuinely believe that he is the best football player ever, even though he barely knows the game, Birmaher said.
Many patients with the early symptoms of bipolar disorder seem to be falling through the cracks. “Some psychiatrists don’t believe the disorder exists, that you can’t have children aged 6 to 12 years old with bipolar disorder. I understand them, because the disorder is hard to diagnose, especially if you don’t ask the right questions and closely follow these children over time,” Birmaher said.
The Pittsburgh Bipolar Offspring Study has been following 388 children of parents with bipolar disorder for more than 16 years. Researchers found that four-fifths of the children who were symptomatic at the outset of the study were not receiving any mental health treatment, despite having ADHD, behavior problems, anxiety, or depression. So far, about 28 percent of the children have developed bipolar disorder, compared with 1 percent of the control group from the same community being studied.
Bipolar disorder is also influenced by a number of environmental risk factors, researchers found, including stressful life events; sexual abuse; antidepressants, which can trigger mania; smoking, which research has shown plays a causal role in mental illness; and substance abuse. Children with very high academic attainment may also be at greater risk for bipolar disorder, according to the review.
Caution Needed With Early Treatment
Choosing preventive medication treatments is particularly complex. The potential benefits of any pre-onset interventions must be carefully weighed against the risks of such treatment, Salagre said. Moreover, patients at risk for bipolar disorder might not convert to the full-blown illness. Pilot studies assessing the protective properties of valproate sodium and quetiapine against the onset of mania have been mixed. Still, some treatments such as lithium are more effective in the earlier stages of the disease, the authors wrote.
“For patients whose prodromal symptoms affect their functioning, you can try treating with the standard treatments for bipolar disorder, but the reality is we don’t know what’s best,” Birmaher said. For now, his treatment strategy is to use evidence-based psychotherapy and/or medication that addresses their presenting symptoms. However, although these young people may present with anxiety or depression, both Salagre and Birmaher cautioned that the standard SSRI treatment can trigger mania. “It’s not necessarily contraindicated, but you need to be super careful when prescribing antidepressants. Parents, too, need to be told what side effects to watch for,” Birmaher said.
The authors recommend cautious use of pharmacotherapy and very gradual dosage escalations. Patients who have an early bad experience with medication may drop out of treatment and resist taking psychotropic drugs for years to come, they noted.
Among the various types of psychotherapy examined, Salagre said family-focused therapy provided longer stability and worked better at reducing symptoms of bipolar disorder than other forms of therapy. Clinicians can also help at-risk patients by screening for stressful life events and encouraging lifestyle modifications, including substance use cessation, physical activity, and healthy diet, she added.
Ultimately, the authors called for more study on the development and identification of treatments that can best prevent or at least delay bipolar disorder, and this “should be considered a priority in psychiatry.” ■
“Early Intervention in Bipolar Disorder” can be accessed here.



