Journal Digest
Women Less Likely to Be Listed First When Co-First Author Is Man

Women co-first authors are less likely to be listed first in a clinical science journal byline, according to an article in JAMA.
Overall, among studies published between 2005 and 2014 in five high-impact clinical journals (Annals of Internal Medicine, BMJ, JAMA, Lancet, and the New England Journal of Medicine), women co-first authors were listed first about 37 percent of the time when a man was the counterpart co-first author. This disproportionality was not seen in the top basic science journals (Cell, Journal of Experimental Medicine, Nature, Nature Medicine, and Science); between 2005 and 2014 women co-first authors were listed first 53 percent of the time.
Women co-first authors were about 18 percent more likely to be listed first when the senior author was also a woman, regardless of the type of science journal.
“It is unclear why differences were seen between clinical and basic science journals,” Erin Aakhus, M.D., M.S.H.P., of the University of Pennsylvania Perelman School of Medicine and colleagues wrote. “Possible factors that were not measured include differences in author seniority or specialty, in the proportion of the total authors who were female, or gender bias.”
Aakhus E, Mitra N, Lautenbach E, Joffe S. Gender and Byline Placement of Co-first Authors in Clinical and Basic Science Journals With High Impact Factors. JAMA. 2018; 319(6):610-611.
Restoring Key Metabolite Improves Brain Function in Mouse Model of Alzheimer’s

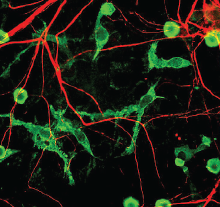
Defects in cellular energy metabolism have been implicated in many neurodegenerative diseases including Alzheimer’s. One factor contributing to this dysfunction may be the depletion of NAD+, a metabolite that helps cells protect against stress and repair DNA damage.
In a study published in Proceedings of the National Academy of Sciences, researchers at the National Institute on Aging and colleagues showed that restoring NAD+ improved outcomes in mice predisposed to develop Alzheimer’s disease (AD).
The study involved mice genetically manipulated to mimic several aspects of Alzheimer’s disease, including abnormal levels of amyloid and tau proteins as well as defective DNA repair mechanisms. The researchers gave some of these mice drinking water with nicotinamide riboside (NR, a form of vitamin B3 and NAD+ precursor) for three months; the others received regular drinking water. Over the next three months, the animals in both groups were evaluated in various behavioral and metabolic tests; during this time the mice in the active group continued to receive NR.
While there was no difference between the groups in amyloid buildup, animals who received chronic treatment with NR had reduced neuroinflammation, tau accumulation, and hippocampal cell death. NR-treated mice also performed better on multiple cognitive tasks than control mice.
“This study suggests that NR/NAD+ can target several aspects of AD, including traditional endpoints like tau pathology and inflammation, maybe via DNA repair enhancement,” the authors concluded. “We believe that this work sets the stage for using NAD+ for treating AD in humans.”
Hou Y, Lautrup S, Cordonnier S, et al. NAD+ Supplementation Normalizes Key Alzheimer’s Features and DNA Damage Responses in a New AD Mouse Model With Introduced DNA Repair Deficiency. Proc Natl Acad Sci USA. 2018; 115(8): E1876-E1885.
Gene Expression Profiles Suggest Similarities, Differences Among Five Psychiatric Disorders
A study led by investigators at the University of California, Los Angeles, has found that gene expression profiles of people with alcohol use disorder, autism, bipolar disorder, major depression, and schizophrenia share several characteristics.
The researchers collected genetic samples from 700 postmortem brains of individuals diagnosed with one of the five psychiatric disorders above as well as samples from 293 brains of healthy individuals and 193 brains from people with inflammatory bowel disease as controls. They then sequenced the samples and compared the expression profiles of over 10,000 genes.
The genetic profiles from patients with autism, bipolar disorder, and schizophrenia showed the most overlap. All three disorders had similar gene expression profiles that indicated synaptic dysfunction and elevated production of astrocytes (a type of non-neuronal support cell in the brain). Autism profiles showed one additional feature: changes in the expression of immune-related brain cells known as microglia.
The profiles of major depression and alcohol use disorder were more distinct.
These findings, published in the journal Science, provide molecular portraits of psychiatric pathology. These genetic signatures act as proxies for brain dysfunction and may lead to more targeted treatments of these disorders.
Gandal M, Haney J, Parikshak N, et al. Shared Molecular Neuropathology Across Major Psychiatric Disorders Parallels Polygenic Overlap. Science. 2018; 359(6376):693-697.
Alcohol Cues May Induce Changes in Brain Glutamate in People With AUD

Growing evidence suggests that glutamate neurotransmission plays an important role in alcohol addiction. A study appearing in the Journal of Alcohol and Alcoholism has now provided the first evidence in humans that glutamate levels in the brain change in response to alcohol-related cues. Alcohol cues (sights or smells related to drinking) are a significant factor that leads to relapse in people with alcohol use disorder (AUD).
Researchers at Indiana University used magnetic resonance spectroscopy to measure forebrain glutamate levels in 17 people with AUD and 18 healthy controls. Two spectroscopy sessions were performed in succession, the first to establish baseline glutamate levels and the second to measure changes in response to different visual cues.
There were no significant differences between the two groups in baseline glutamate levels on average. When presented with visual cues, glutamate levels in the AUD subjects dropped after they were shown alcohol-related photos, but not neutral photos; the control subjects showed no differences in glutamate levels in response to the cues.
“This is the first study to document changes in glutamate levels during exposure to alcohol cues in people with alcohol use disorders and shines a spotlight on glutamate levels as an important target for new therapies to treat the condition,” said study co-author Sharlene Newman, Ph.D., in a press release. ■
Cheng H, Kellar D, Lake A, et al. Effects of Alcohol Cues on MRS Glutamate Levels in the Anterior Cingulate. Alcohol Alcohol. January 10, 2018. [Epub ahead of print]



