U.S. Seniors Matching to Psychiatry Increases For Sixth Straight Year
Abstract
An expanding Match program, increasing competitiveness for residency slots, and the growing attractiveness of psychiatry account for a sharp increase in U.S. graduates matching into psychiatry programs.
A total of 982 U.S. senior medical school students matched with a psychiatry residency in this year’s National Resident Matching Program (NRMP), up from 923 in 2017.
This marks the sixth straight year in which psychiatry’s numbers have risen—the last three years have seen dramatic increases—reflecting a number of trends: the increasing attractiveness of the profession, the growth of the Match itself, and mounting competitiveness for slots, causing some residents to apply in more than one specialty.
But the growth is good news, especially in light of the many areas of the country that are experiencing a severe shortage of psychiatrists.
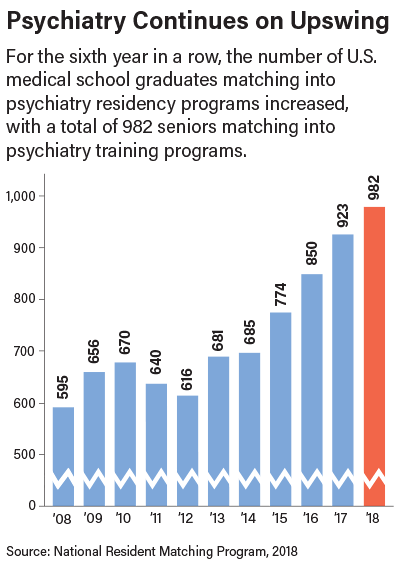
The numbers of U.S. medical school seniors choosing psychiatry has grown somewhat steadily since the mid-1990s when psychiatry’s Match numbers were in the mid-400s. There was some waxing and waning between 2007 and 2012, followed by six years of increasing numbers; in the last four years the number of U.S. medical school seniors matching into psychiatry has gone from 685 in 2014 to this year’s 982 (see chart).
“We are definitely seeing a trend as psychiatry becomes increasingly integrated with the rest of medicine,” said APA President Anita Everett, M.D. “There is a continuing shortage of psychiatrists, so this year’s match is good news for our profession and for our patients.”
APA Director of Education Tristan Gorrindo, M.D., noted that the number of U.S. medical school seniors entering psychiatry is now comparable to many traditionally popular medical specialties such as surgery (1,005 U.S. seniors) and OB/GYN (1,051 seniors).
APA CEO and Medical Director Saul Levin, M.D., M.P.A., said that APA efforts to reach out to medical schools and to mentor young physicians is proving successful. “Our profession is attractive to young doctors who want to treat the whole person—mind, body and brain,” he said. “We welcome new trainees to the profession and invite residents to explore membership in APA.”
Match Numbers Stoke Competitiveness
The Match results are watched with interest as an indicator of the future physician workforce. For applicants, the residency match process begins in the fall during the final year of medical school, when they apply to the residency programs of their choice.
Throughout the fall and early winter, applicants interview with programs. From mid-January to late February, applicants and program directors rank each other in order of preference and submit the preference lists to NRMP, which processes them using a computerized mathematical algorithm to match applicants with programs.
Of the first-year positions offered, 14,695 were in the primary care specialties of family medicine, internal medicine, internal medicine–pediatrics, internal medicine–primary, and pediatrics. Since 2014, the number of primary care positions has grown by 1,713, a 13.2 percent increase.
The number of Match registrants was the highest ever, at 43,909. According to NRMP, the increase was due primarily to graduates of U.S. osteopathic medical schools. The number of U.S. osteopathic medical school students and graduates who submitted program choices was 4,617; 3,771 (81.7 percent) matched to PGY-1 positions. Both are all-time highs, according to NRMP.
Since 2014, the number of U.S. osteopathic medical school students and graduates seeking positions has risen by 1,879, a 68.6 percent increase. Participation by osteopathic students is expected to continue to grow over the next several years as a result of the transition to a single accreditation system; by 2020, when all graduate medical education programs are accredited by the ACGME, the American Osteopathic Association Match will cease to exist.
Number of IMG Participants Declines
One category of medical graduates participating in the overall Match that declined is non-U.S. citizen international medical graduates (IMGs)—a phenomenon that may reflect increasing uncertainty about the status of immigrants under the Trump administration. In 2018, 7,067 IMGs submitted program choices, down from 7,284 in 2017 and 7,460 in 2016.
At the same time, however, 3,962 IMGs (56.1 percent) matched to first-year positions, the highest match rate since 1993. Moreover, IMGs—whether American or non-U.S. citizen—continue to be critical to psychiatry. A total of 1,556 psychiatry positions were offered, of which 1,540 were filled; 982 were filled by U.S. medical school seniors, so the rest were filled by American and non-U.S. citizen IMGs; osteopaths; and American graduates from previous years.
Educators at medical schools and training programs across disciplines say growing Match numbers create an impression of mounting competitiveness. They say graduates—driven by acute anxiety about being accepted into a training program after having already accumulated considerable medical school debt and the perception of greatly heightened competitiveness—are applying to and interviewing at more and more programs.
“Senior medical students, aware of the limited number of residency positions in sought-after specialties, are considering more options as they plan their medical careers,” said Sidney Weissman, M.D., a former APA trustee with a longtime interest in workforce issues. “This is why many of us have interviewed applicants applying in more than one specialty. This occurs because students, heeding the advice of medical school deans to apply to more than one specialty, believe there are reduced training opportunities.”
(Funding of graduate medical education through the Medicare program has been capped since 1997, freezing the number of training positions at institutions funded with federal dollars. Programs that had not previously received federal funds are eligible for new federal dollars, but these programs account for only a small increase in the number of residency slots. Some funding to support more positions is supplied by states and—in rare instances—individual hospitals.)
Statistics from the Electronic Residency Application Service, through which students can apply to programs online, document a significant growth in applicants to residency programs in the last decade. Between 2007 and 2017, the number of applicants to psychiatry training programs increased 73 percent (see Psychiatric News, January 27, 2017). ■
More information about the 2018 National Resident Matching Program can be accessed here.



