Journal Digest
Infrared Spectroscopy Can Visualize Post-Concussive Brain Problems

An imaging technique known as functional near-infrared spectroscopy (fNIRS) may be able to detect differences in the brains of people with and without post-concussion symptoms, suggests a study in the Journal of Neurotrauma.
The researchers measured the brain activity of 12 patients with post-concussion symptoms at rest and when performing a range of cognitive tasks. They compared this activity to that of 12 healthy controls performing similar tasks. The fNIRS images showed that the patients with post-concussion symptoms had reduced connectivity between their right and left dorsolateral prefrontal cortex, particularly during a working memory task. The degree of connectivity reduction also correlated with symptom severity.
“[M]ore research is needed to evaluate if fNIRS interregional coherence could be an objective aid for monitoring TBI,” the authors wrote. “fNIRS measures of coherence may provide a useful biomarker of injury and recovery, adding to our understanding of the pathophysiology of [mild TBI] and providing a new method to assess treatment responses.”
Hocke L, Duszynski C, Debert C, et al. Reduced Functional Connectivity in Adults With Persistent Post-Concussion Symptoms: A Functional Near-Infrared Spectroscopy Study. J Neurotrauma. March 23, 2018. [Epub ahead of print]
Disordered Eating Behavior In Youth May Increase Risk Of Depression
Youth who display behavior commonly associated with eating disorders may be at a greater risk of depressive symptoms and bullying by peers, according to a study in JAMA Psychiatry. Disordered eating behavior includes such actions as eating in secret or purposefully vomiting after a meal.
The findings suggest that “interventions to treat disordered eating behavior could prove to be beneficial for reductions in depressive symptoms and problematic peer relations,” wrote study authors Kirsty S. Lee, Ph.D., and Tracy Vaillancourt, Ph.D., of the University of Ottawa. “Interventions for disordered eating behavior should ideally target negative attitudes, promote healthy weight control behavior, and contain an element of self-compassion, which can reduce symptoms of disordered eating and other psychopathologic symptoms.”
To examine the concurrent and long-term relationship between bullying by peers, disordered eating behavior, and symptoms of depression, Lee and Vaillancourt analyzed data from the McMaster Teen Study—a longitudinal study that has been collecting information about bullying and mental health in youth annually since 2008 (when the participants were in 5th grade, or about 10 years old). The current analysis focused on data collected from students in grades 7 through 11 (aged 13 to 17).
A total of 612 students completed annual online or paper questionnaires, which asked them to gauge how often they experienced bullying at school, engaged in disordered eating behavior, and felt depressed.
A statistical model used by the authors revealed that “bullying by peers was concurrently associated with disordered eating behavior and depressive symptoms at every time point during the five-year period,” they reported. The model also revealed that disordered eating behavior was associated with increases in depressive symptoms in the following year.
Longitudinal Associations Among Bullying by Peers, Disordered Eating Behavior, and Symptoms of Depression During Adolescence. JAMA Psychiatry. April 11, 2018. [Epub ahead of print]
Gender-Affirming Hormones Pose No Significant Safety Risks in Youth

Many transgender youth undergo hormonal therapy so their physical gender more closely aligns with their gender identity. However, little is known about the safety and impact of gender-affirming hormones in this young population.
A prospective study published in the Journal of Adolescent Health reports that while hormonal therapy results in significant physiological changes, almost none of these changes led to any safety concerns over a two-year period.
The investigators, led by a group at Children’s Hospital in Los Angeles, enrolled 101 youth and young adults (aged 12 to 23) who were planning to undergo gender transition and followed them for 21 to 31 months. At the end of the follow-up period, data were available for analysis on 25 transfeminine and 34 transmasculine participants.
The transfeminine youth showed statistically significant changes in the levels of high-density lipoprotein (HDL), aspartate aminotransferase, potassium, prolactin, and hemoglobin at follow-up. Transmasculine youth experienced statistically significant changes in blood pressure, HDL, triglycerides, aspartate aminotransferase, alanine aminotransferase, potassium, and hemoglobin levels. Except for some instances of blood pressure elevation in transmasculine youth, none of these changes required any clinical intervention.
“As the demand for care continues to exponentially increase across the United States, much more data are needed about the impact of hormonal therapy on both the physical and mental health in transgender adolescents,” the authors concluded.
Olson-Kennedy J, Okonta V, Clark L, Belzer M. Physiologic Response to Gender-Affirming Hormones Among Transgender Youth. J Adolesc Health. 2018; 62(4):397-401.
Meta-Analysis Suggests Aripiprazole Switching Does Not Worsen Psychosis
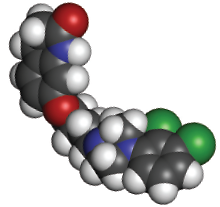
Numerous case reports have reported a worsening of psychosis symptoms in schizophrenia patients who have switched to aripiprazole or added it to other medications. A meta-analysis published in the Journal of Clinical Psychiatry suggests that introducing aripiprazole is not associated with psychosis worsening, though it may increase the odds of discontinuing medication.
Investigators at the Centre for Addiction and Mental Health in Toronto identified and reviewed 22 randomized, controlled trials (5,769 total patients) that assessed psychotic worsening related to aripiprazole treatment; 13 studies involved patients who switched to aripiprazole from another antipsychotic, while nine studies involved patients who added aripiprazole to their existing treatments.
The analysis showed no significant difference in the risk of psychotic worsening between switching to aripiprazole and switching to another antipsychotic. However, switching to aripiprazole was related to about a 46 percent greater risk of study discontinuation due to lack of efficacy. There wre not enough data to make conclusive results about the clinical risks of adding aripiprazole to existing treatments.
Takeuchi H, Fathi A, Thiyanavadivel S, et al. Can Aripiprazole Worsen Psychosis in Schizophrenia? A Meta-Analysis of Double-Blind, Randomized, Controlled Trials. J Clin Psychiatry. 2018; 79(2): 17r11489.
Researchers Visualize Microglia in Action For First Time
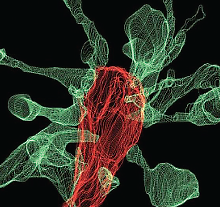
Microglia are support cells in the brain that help guide the healthy development of neurons. One role of microglia is to prune damaged or unnecessary connections (synapses) between neurons—though until now this process has never actually been visualized.
A joint research team from the European Molecular Biology Laboratory (EMBL) in Rome and EMBL Heidelberg used advanced time-lapse microscopy to capture microglial pruning on video.
Their findings, which were published in Nature Communications, reveal that while microglia can “chew up” synapses, they do so in a more delicate and nuanced fashion than was previously believed. This finding may help researchers better understand synapse remodeling, which is particularly active during adolescence. Dysfunctional synaptic remodeling is believed to be associated with mental disorders such as schizophrenia.
The microscopy revealed that microglia do not simply undertake phagocytosis, which engulfs entire synapses. Instead, these cells gently “nibble” on certain synaptic structures—a process known as trogocytosis. This nibbling appeared to be restricted to structures on the presynaptic end of the connection (the side that sends out chemical signals); the receiving end, or postsynaptic terminal, was unaffected.
The EMBL team also observed that when microglia contacted synapses, they induced the formation of thin strands known as filopodia. These strands are involved in seeking out potential new connections, which suggests that in addition to pruning back some structures, microglia assist in synaptic growth as well. ■
Weinhard L, di Bartolomei G, Bolasco G, et al. Microglia Remodel Synapses by Presynaptic Trogocytosis and Spine Head Filopodia Induction. Nat Commun. 2018; 9(1):1228.



