Arkansas Medicaid Work Requirement Led to Coverage Losses, Study Shows
Abstract
There was no change in employment or community engagement as a result of the work requirement largely because nearly all of the targeted population had an exemption or was already meeting the requirements, according to the lead investigator.
Medicaid coverage of low-income Arkansas residents between 19 and 34 years of age dropped by almost 7% after the state instituted work requirements for Medicaid beneficiaries, while lack of any insurance among the same group rose by 4%.
At the same time, there were no significant gains in employment or in community engagement by beneficiaries, and many beneficiaries were unaware of the policy or were unsure how to comply with the requirements.
These were among the findings of a telephone survey of 5,955 low-income individuals in Arkansas and three comparison states (Kentucky, Louisiana, and Texas) published September 12 in The New England Journal of Medicine (NEJM). Not all of the respondents were Medicaid beneficiaries; some may have had Obamacare, another kind of insurance, or no insurance.
The survey results appear to support claims by APA and other health organizations that work requirements will lead to health coverage losses.
In June 2018, Arkansas became the first state to implement work requirements in Medicaid. The state notified beneficiaries aged 30 to 49 that they were required to work 80 hours a month, participate in another qualifying community engagement activity such as job training or community service, or meet criteria for an exemption such as pregnancy or disability.
By December, nearly 17,000 adults were notified by mail that they had been removed from Medicaid. In March 2019, a federal judge halted the program owing to concerns about its effect on coverage (Psychiatric News).
According to the Kaiser Family Foundation Medicaid Waiver Tracker, other states have submitted waivers to implement work requirements—Alabama, Mississippi, Oklahoma, South Carolina, South Dakota, Tennessee, and Virginia—and others have been approved for such changes: Arizona, Indiana, Michigan, Ohio, Utah, and Wisconsin. A work requirement waiver in Kentucky was also halted by the federal court in March; it is being challenged again in appeals court, where APA has joined in an amicus brief arguing that the waiver will be especially harmful to patients with serious mental illness (Psychiatric News).
“More than a dozen states have proposed work requirements in Medicaid, but Arkansas is the only one that fully implemented them [before the court stepped in earlier this year],” Benjamin D. Sommers, M.D., Ph.D., lead author of the NEJM report, told Psychiatric News. “While advocates of the policy say it can increase employment, raise people out of poverty, and replace Medicaid coverage with private insurance, we don’t find any evidence of those changes and instead see people losing their health insurance largely due to red tape.”
Sommers is a professor of health policy and economics at the Harvard T. H. Chan School of Public Health and Brigham and Women’s Hospital.
The researchers conducted a random-digit dialing telephone survey to compare changes in outcomes before and after implementation of the work requirements in Arkansas among people aged 30 to 49, as compared with Arkansans aged 19 to 29 and 50 to 64 (who were not subject to the requirement in 2018) and with adults in the three comparison states.
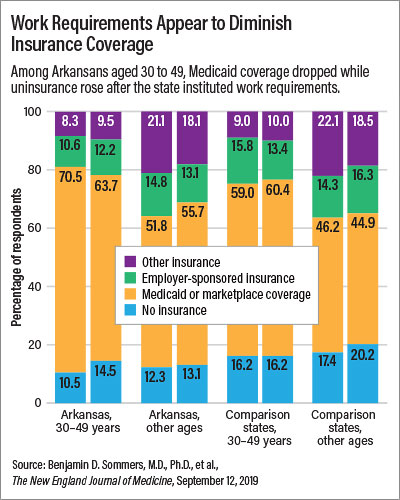
Sommers and colleagues found that the share of Arkansans aged 30 to 49 who had Medicaid or marketplace coverage under the Affordable Care Act went from 70.5 percent in 2016 to 63.7 percent in 2018. Meanwhile, the percentage of uninsured respondents among Arkansans aged 30 to 49 increased from 10.5% in 2016 to 14.5% in 2018 (see chart above).
In all groups and comparison states, employment declined between 2017 and 2018; among Arkansas residents aged 30 to 49, employment declined by 3.5 percentage points, from 42.4% to 38.9%.
“Implementation of the work requirements led to significant losses of Medicaid and an increase in the share of adults without any health insurance in the age range targeted by the policy,” Sommers said. “There was no significant change in employment or any of the other community engagement activities that the policy requires—primarily because 97% of the target population already met the requirements, based primarily on working or having a disability.”
Moreover, Sommers and colleagues also found that nearly a third of respondents aged 30 to 49 were unaware of the policy change, and more than half indicated they were unsure if it applied to them or not.
“Even those who knew about it were often confused about how it worked or what they had to do to keep their insurance coverage,” Sommers said. “This is the most likely reason why there were significant coverage losses even though most people were already meeting the requirements in one way or another.”
He concluded, “These results should serve as a strong note of caution to states moving ahead with work requirements, which may not have their desired effects.” ■



