Opioid Misuse on the Decline, But More Adults Using Marijuana
Abstract
The 2018 National Survey on Drug Use and Health highlights both positive trends and areas for improvement in the treatment and prevention of substance use and mental health disorders.
The number of Americans who misused prescription opioid pain relievers within the previous year fell 11% from 2017 to 2018, a difference of more than 1.2 million people, according to the 2018 National Survey on Drug Use and Health (NSDUH).
The NSDUH, published by the Substance Abuse and Mental Health Services Administration (SAMHSA) each year, is a comprehensive survey of approximately 67,500 civilian, noninstitutionalized people aged 12 or older; the results are extrapolated to the U.S. population. It covers substance use, substance use disorders, mental health, and the receipt of related treatment services.
The decline in prescription opioid pain relievers was accompanied by a small but significant drop in heroin use, which had begun to decline in 2017. The number of people who received medication treatment for opioid use disorder increased, from roughly 1.03 million to roughly 1.2 million.
However, the number of Americans who used marijuana in the previous year jumped 15%, a difference of roughly 5.5 million people. The large increase in marijuana use occurred primarily in adults older than 26 years, with the number of adults in this population who reported using marijuana in the past month increasing from 7.9% in 2017 to 8.6% in 2018, a difference of 1.7 million people.
Levels of past-month use in adolescents aged 12 to 17 years and young adults aged 18 to 25 years remained stable at roughly 6.7% and 22.1%, respectively. Frequent marijuana use in both youth and young adults appears to be associated with risk for opioid use, heavy alcohol use, and major depressive episodes.
Other key findings of the report include the following:
Past-month cocaine use declined significantly among young adults, from 1.9% to 1.5%.
Past-year methamphetamine use dropped from 1.1% to 0.8% in young adults, but rose from 0.6% to 0.7% in adults aged 26 years and older.
Past-year misuse of prescription stimulants dropped in young adults from 7.4% to 6.5%.
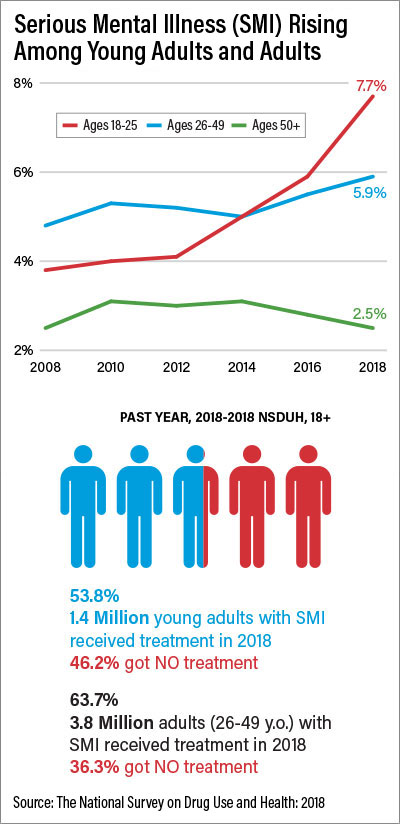
The percentage of adolescents who experienced a major depressive episode in the past year rose from 13.3% to 14.4%, while the percentage of young adults who experienced a major depressive episode in the past year rose from 13.1% to 13.8%.
11% of young adults had serious thoughts of committing suicide in the previous year.
Nearly 90% of people older than 12 years who have a substance use disorder did not receive treatment.
Nearly 57% of adults aged 18 years or older who have any mental illness did not receive treatment.
“The NSDUH data provide a foundation that helps to focus resources to address the important areas of mental health and substance use issues in our nation,” said psychiatrist Elinore McCance-Katz, M.D., Ph.D., the assistant secretary for mental health and substance use and head of SAMHSA. “I am especially pleased to see that our prevention efforts appear to be working, and we will continue to deliver those important messages.” ■
The NSDUH report is posted here.



