Journal Digest: Children of Refugees; Theta Burst Stimulation; Chromosomes in Brain Cells
Children of Refugees With PTSD Have Greater Risk of Psychiatric Illness

A study using Danish health and immigration data found that the children of refugees diagnosed with posttraumatic stress disorder (PTSD) are at greater risk of mental illness than refugee children whose parents did not have PTSD. This elevated risk was present even if the children were born after their parents settled in Denmark.
The findings highlight “a major public health challenge in the countries in which refugees seek asylum for decades to come,” wrote the authors of the study, which was published in Lancet Public Health. “[T]he numbers of children of refugee parents will probably rise as a result of the displacement of millions of refugees, particularly to western Europe, since 2014.”
Researchers from the University of Copenhagen and colleagues assessed the health outcomes of 51,793 children of refugees who either arrived or were born in Denmark prior to January 2016. Of these children, 7,486 had at least one parent with PTSD.
Having a parent with PTSD significantly increased the risk that a refugee child would be diagnosed with a psychiatric disorder by the age of 18. For instance, children whose father had been diagnosed with PTSD were 1.5 times as likely to be diagnosed with psychiatric disorder than those who did not have a parent with PTSD. The risk of a psychiatric diagnosis was higher still in children with a mother with PTSD (1.6 times as likely) and children who had two parents with PTSD (1.8 times as likely).
Children born in Denmark whose refugee parents had PTSD had a lower risk of a psychiatric diagnosis by age 18 than those who arrived as refugees along with their parents; however, these children had a significantly elevated risk of a psychiatric diagnosis compared with children of refugees who did not have PTSD.
Back Nielsen M, Carlsson J, Køster Rimvall M, et al. Risk of Childhood Psychiatric Disorders in Children of Refugee Parents With Posttraumatic Stress Disorder: A Nationwide, Register-based, Cohort Study. Lancet Public Health. 2019; 4(7): e353-e359
New Theta Burst TMS Is Cost-Effective

Intermittent theta burst stimulation (iTBS) is a new form of transcranial magnetic stimulation (TMS) in which individual treatment sessions can be done in three minutes instead of 30 minutes to 40 minutes. A study published in PLoS One reports that this shorter treatment duration can translate into cost savings for patients.
Researchers at the University of Toronto and colleagues used data from a large clinical study that compared the effects of iTBS and repetitive TMS (or rTMS) on depression symptoms. Based on the number and length of treatment sessions each patient underwent, the researchers estimated the cost of each procedure in a typical clinic that was open eight hours a day.
Participants in both groups underwent an average of 26 sessions. On average, a course of iTBS therapy cost $1,108 per patient, while a course of rTMS cost $1,844. According to the authors, the lower cost of iTBS was due to lower costs for technician time and operation of the magnetic coils. The costs of physician assessment remained the same for both types of TMS and represented the bulk of costs for iTBS.
About 30% of patients in both TMS groups achieved remission of their depressive symptoms in this clinical study. Thus, the average cost per remission still significantly favored iTBS ($3,695 versus $6,146).
Mendlowitz AB, Shanbour A, Downar J, et al. Implementation of Intermittent Theta Burst Stimulation Compared to Conventional Repetitive Transcranial Magnetic Stimulation in Patients With Treatment Resistant Depression: A Cost Analysis. PLoS One. 2019; 14(9): e0222546
Scientists Take Closer Look at Chromosomes in Brain Cells
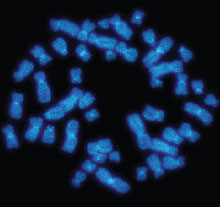
How chromosomes fold together, along with the position of their epigenetic markers (chemical tags added to DNA at specific locations), regulates which genes are turned on or off in a cell. A study appearing in Nature Methods details a new automated technique that can simultaneously analyze the 3-D shape of chromosomes within brain cells and their epigenetic profile.
Researchers previously have had to conduct folding and epigenetic experiments separately, limiting their ability to understand how these two forms of gene regulation interact in the same cell. The new approach—known as single-nucleus methyl-3C sequencing—may help researchers better understand how brain cells might become dysregulated and ultimately contribute to mental illness. This technique was developed by researchers at the Salk Institute.
The Salk researchers tested their method on more than 4,200 human brain prefrontal cortex cells. The automated sequencing tool enabled them to separate out 14 distinct types of cells (neurons and non-neurons), as each had a unique 3-D and epigenetic profile. A comparison of the different cell profiles confirmed the hypothesis that these two regulatory mechanisms interact extensively.
With the basic methodology now established, the researchers noted that the next step will be to conduct single-nucleus methyl-3C sequencing on both healthy and diseased brain cells. ■
Lee DS, Luo C, Zhou J, et al. Simultaneous Profiling of 3D Genome Structure and DNA Methylation in Single Human Cells. Nat Methods September 9, 2019. [Epub ahead of print]



