Methamphetamine Involved in Rising Number of Heroin Treatment Admissions
Abstract
In a trend that cuts across demographics, adolescents and young adults are among the groups hardest hit.
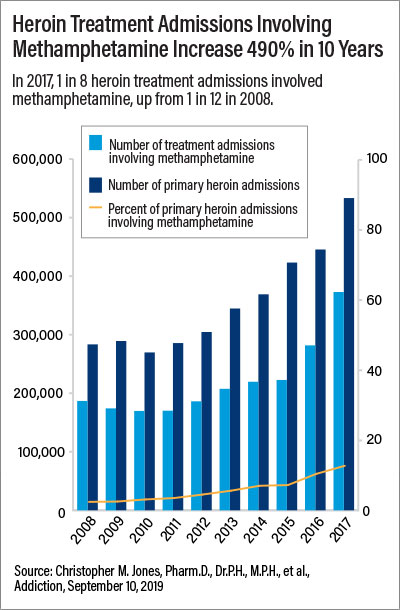
Methamphetamine use is involved in an increasing number of heroin treatment admissions, a study in Addiction has found. In 2017, 12.4% of heroin treatment admissions involved methamphetamine, up from 2.1% in 2008. The trend was pronounced in adolescents and young adults but also cut across sex, age, race, ethnicity, and census regions nationwide.

Treatment plans for patients who use heroin and methamphetamine should include medication treatment for opioid use disorder, says Christopher M. Jones, Pharm.D., Dr.P.H., M.P.H.
The findings point to a need for more dialogue between health professionals and patients about using multiple substances, lead author Christopher M. Jones, Pharm.D., Dr.P.H., M.P.H., told Psychiatric News. Jones is a senior advisor and the associate director of the Office of Strategy and Innovation in the Injury Center at the Centers for Disease Control and Prevention.
“Clinicians should discuss with their patients not only opioid use, but also methamphetamine and other substance use. These drugs work in different ways, and prior research indicates that there are varying motivations for their combined use. These include synergistic euphoric effects or balancing effects, such as using methamphetamine to counter the sedating effects of opioids,” Jones told Psychiatric News. “Understanding why patients are using methamphetamine in addition to opioids can help guide decisions related to treatment and recovery-support services.”
Prompted by reports of increased rates of simultaneous opioid and methamphetamine use, Jones and his colleagues analyzed data from more than 3.5 million treatment admissions between 2008 and 2017 in which heroin was the primary substance of use. The data came from the Treatment Episode Data Set, a national database that provides information on the admissions of people aged 12 years and older to substance use treatment centers that receive federal funds.
“There were a small number of local studies that had come out in the last two years that started to document this phenomenon. We were interested to see what the patterns looked like in a larger dataset as the findings could help to inform ongoing efforts to combat the evolving opioid overdose epidemic,” Jones said.
The researchers found that in 2017, people aged 12 to 24 had the highest rates of admissions for heroin use involving methamphetamine of all the age groups examined: 27.8% of primary heroin treatment admissions for adolescents aged 12 to 17 years involved methamphetamine, and 17.4% of heroin treatment admissions for young adults aged 18 to 24 involved methamphetamine.
“Not only do these findings highlight a need to focus intervention and treatment efforts aimed at reaching younger age groups, but together with the finding that early age of heroin initiation was associated with methamphetamine use at treatment admission, these findings underscore the importance of expanding policies, programs, and practices that can prevent initiation of these substances in the first place,” Jones and colleagues wrote.
Among females, 15.1% of primary heroin treatment admissions involved methamphetamine in 2017, compared with 10.8% among males. The researchers noted that prior research suggests that females use more methamphetamine and transition from recreational use to dependence more quickly than males.
More than 37% of primary heroin treatment admissions among non-Hispanic American Indian or Alaska Natives involved methamphetamine, the highest among all races and ethnicities. Only 2% of primary heroin treatment admissions among non-Hispanic black people involved methamphetamine, the lowest among all races and ethnicities.
“Given the increase in risk for negative health outcomes among people using both substances, comprehensive prevention, treatment, and harm-reduction strategies that address the polysubstance nature of opioid use and are appropriately tailored to specific demographic groups and at-risk populations are needed,” Jones and colleagues wrote.
Yet despite the greater risk of poor outcomes in people who mix illicit opioids with other drugs, admissions for the use of heroin and methamphetamine are 35% less likely to include medication treatment for opioid use disorder as part of the treatment plan, the study revealed.
“Ensuring that the patient treatment plan utilizes evidence-based medications for opioid use disorder treatment along with nonmedication services, especially those that have shown benefit for patients using methamphetamine, is essential,” Jones said. “In addition, given the high risk for overdose among this population, patients should be given or prescribed naloxone for opioid-overdose reversal and trained in its use.” ■
“Increases in Methamphetamine Use Among Heroin Treatment Admissions in the United States, 2008-2017,” is posted here.



