Journal Digest: Smoking Ban; Breath Collection; Flibanserin; Light Flash Therapy; Brain Imaging
Smoking Ban in MH Settings Reduces Conflicts Between Staff, Patients

Adopting a comprehensive smoke-free policy in psychiatric hospitals may reduce conflict between patients and staff, according to a study in the International Journal of Mental Health Nursing.
Researchers at Kings College London and colleagues examined rates of smoking-related incidents at a psychiatric hospital in London in the 12 months before and after the facility became smoke-free in 2014. Prior to this, smoking was not permitted inside the hospital, but patients could take occasional smoke breaks outside.
They identified 61 smoking-related incidents in the year prior to the policy change, and 32 incidents in the year following the change. Reports of patients being confrontational with staff after being approached about the hospital’s smoking policy rose slightly after the policy change; however, these incidents were offset by the elimination of confrontations during smoke breaks and a reduction in incidents when patients were denied a smoke break by staff.
“We have demonstrated that designated smoking breaks are a source of conflict … and for the first time shown that eliminating breaks as part of a comprehensive smoke-free policy may remove this source of conflict,” the authors wrote.
Spaducci G, McNeill A, Hubbard K, et al. Smoking-Related Violence in a Mental Health Setting Following the Implementation of a Comprehensive Smoke-Free Policy: A Content Analysis of Incident Reports. Int J Ment Health Nurs. September 12, 2019. [Epub ahead of print]
Researchers Develop Opioid Analyzer Using Breath Collection

Scientists may be one step closer to identifying a noninvasive way to detect opioids in patients. A pilot study of patients with chronic pain at the University of California, Davis, suggests opioid metabolites can be detected and quantified from exhaled breath.
“Techniques that monitor exhaled drugs in breath are relatively new, and most of them are in the early stages of development. However, the use of breath drug-monitoring platforms is very attractive in terms of being noninvasive and useful in a variety of settings,” the researchers wrote. “Exhaled breath collection represents a painless, easily available, and noninvasive technique that would enable clinicians to make quick and well-informed decisions.”
For this pilot study, the researchers collected breath samples from 10 adults—seven patients undergoing pain management treatment with intravenous opioids and three controls not taking opioids. Six of the pain patients were also taking oral oxycodone, while one was taking oral methadone. The participants provided samples by exhaling into a dry ice–filled container that quickly condenses the breath for analysis. Each participant provided two breath samples about 60 to 90 minutes apart, with a blood draw taken immediately afterward.
Using mass spectrometry, the researchers were able to identify opioid metabolites that reflected the medication the patients were taking. Though the metabolites were present at lower levels than in corresponding blood samples, there was a correlation between the relative breath and blood concentrations of each patient.
“[T]he small number of subjects precludes any robust conclusions, and more subjects taking a specific opioid and at various times from opioid ingestion will be required,” the researchers wrote. Additional studies with larger samples will also be needed to see how sex, weight, and metabolism influence the breath analysis, they added.
The study was published in the Journal of Breath Research.
Borras E, Cheng A, Wun T, et al. Detecting Opioid Metabolites in Exhaled Breath Condensate (EBC). J Breath Res. 2019; 13(4): 046014
Flibanserin Found to Be Safe When Taken Hours After Drinking

Flibanserin—a medication approved for some types of hypoactive sexual desire disorder (HSDD) in premenopausal women—is safe if taken two or more hours after drinking alcohol, two studies in the Journal of Sexual Medicine suggest. The findings support the recent decision by the Food and Drug Administration (FDA) to change the label of flibanserin from recommending women taking the medication avoid alcohol (due to the risk of low blood pressure and fainting) to recommending that women discontinue drinking alcohol at least two hours before taking the medication.
To assess the potential physiological interactions of alcohol and flibanserin, researchers at George Washington University and colleagues conducted two small clinical studies involving healthy premenopausal women (who were not assessed for HSDD). In one study, 64 women consumed either orange juice or orange juice plus alcohol (the equivalent of two glasses of wine) prior to taking 100 mg flibanserin two, four, or six hours later or a placebo pill two hours later. Each woman participated in eight drinking sessions over two weeks, though the order was assigned randomly.
Overall, there was no statistical difference in the rates of hypotension (defined as systolic blood pressure <90 mm Hg and diastolic blood pressure <60 mm Hg) when women received flibanserin compared with when they received placebo. There was only one incident of fainting, and that was a participant who took placebo four hours after consuming alcohol.
In the other study, 24 women were assigned to receive either 100 mg flibanserin or placebo at bedtime 2.5 hours after consuming a three-course dinner and two glasses of wine. As with the other study, there was no difference in the rate of hypotension or adverse events such as dizziness or fainting in women who took flibanserin or placebo at bedtime.
These studies were funded by Sprout Pharmaceuticals, the manufacturer of flibanserin.
Simon JA, Clayton AH, Kingsberg SA, et al. Effects of Timing of Flibanserin Administration Relative to Alcohol Intake in Healthy Premenopausal Women: A Randomized, Double-Blind, Crossover Study. J Sex Med September 12, 2019. [Epub ahead of print]
Millheiser L, Clayton AH, Parish SJ, et al. Safety and Tolerability of Evening Ethanol Consumption and Bedtime Administration of Flibanserin in Healthy Premenopausal Female Subjects. J Sex Med September 10, 2019. [Epub ahead of print]
Light Flash Therapy Coupled With CBT Can Improve Sleep

Light flash therapy combined with cognitive-behavioral therapy (CBT) can improve sleep in adolescents, according to a study published in JAMA Network Open. Light flash therapy is a technique in which ultra-brief (millisecond) flashes of bright light are pulsed during sleep; these flashes can be processed by the retina, which in turn can adjust circadian rhythms.
In this two-phase study, researchers at Stanford University and colleagues enrolled 102 adolescents aged 14 to 18 who reported difficulty going to bed early and waking up early. In the first phase, 72 adolescents were assigned to receive either active light therapy (3 millisecond pulses every 20 seconds for three hours) or sham light (3 millisecond pulses every 20 seconds but only for one minute each hour) nightly for four weeks. The second phase was similar, but all 30 participants also received four weekly sessions of CBT. The light flash duration was also reduced from three hours to two hours, as some participants reported the lights to be disruptive.
There were no differences in sleep and wake times as reported in sleep diaries or subjective measures of sleep quality between adolescents who received active or sham light therapy in phase one. In the second phase, however, the adolescents receiving CBT in addition to light flash therapy reported getting to bed about 50 minutes earlier and sleeping for 43 minutes longer on average relative to those receiving sham light.
Kaplan KA, Mashash M, Williams R, et al. Effect of Light Flashes vs Sham Therapy During Sleep With Adjunct Cognitive Behavioral Therapy on Sleep Quality Among Adolescents: A Randomized Clinical Trial. JAMA Netw Open. 2019; 2(9): e1911944
Brain Imaging May Predict Exposure Therapy Response in OCD Patients
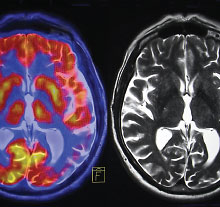
Brain imaging may be able to predict which patients with obsessive-compulsive disorder (OCD) will benefit from exposure therapy, according to a study published in PNAS.
Researchers at Columbia University and colleagues asked 36 adults with OCD and 33 controls without OCD to complete the Simon Spatial Incompatibility Task while receiving a functional MRI (fMRI) scan. This task involves identifying which way a left or right arrow that quickly appears on the left or right side of a screen is pointing. The task is designed to assess conflict control, as the participant must disregard the spatial direction and focus on the arrow direction. The researchers chose this task since it is believed that OCD symptoms reflect the brain’s inability to resolve cognitive conflicts.
After completing the task, all OCD participants were offered 17 twice-weekly sessions of exposure therapy; 17 of the patients achieved remission following therapy. The researchers identified a pattern of elevated brain activity in several regions among people who responded to treatment. These regions included the left pallidum (which controls voluntary movements), the visual cortex, and several small regions linked with the default mode network (which is active when people are daydreaming). By using this pattern as a template, the researchers could predict which patients responded to therapy with about 80% accuracy.
“[T]hese results represent an important step toward targeting treatment plans to specific patients, while suggesting that improving the capacity to resolve cognitive conflict may be a target for novel treatments,” the authors wrote. ■
Pagliaccio D, Middleton R, Hezel D, et al. Task-based fMRI Predicts Response and Remission to Exposure Therapy in Obsessive-Compulsive Disorder. Proc Natl Acad Sci USA. September 23, 2019. [Epub ahead of print]



