Journal Digest
Adolescents With Autism Appear Less Influenced By Advice of Others
The opinions of others can influence decision making, but a study published in PNAS reports that such social influence differs between children with autism and typically developing children.
For the study, researchers from the University of Oxford invited 125 typically developing children between the ages of 6 and 14 to play a videogame in which they were required to navigate a spaceship around a series of black holes. Before each important navigation point, the children saw a video of either a child or an adult who would provide advice (which could be correct or incorrect) on how best to accomplish this task. A smaller cohort of 30 children with autism (matched by age and IQ) also performed this task under identical circumstances.
Whereas adolescents aged 12 to 14 showed a bias to listen to the advice (regardless of whether the advisor was an adult or child and/or the advice given was good or bad), children under 12 did not. In contrast, the children with autism were not significantly influenced by the advice of others at any age. As a result, older children with autism performed better on the navigation task than their neurotypical peers.
Though the sample size of children with autism was small, the researchers said these findings suggest that age 12 is a key period of divergence in how the brain integrates social cues.
Large I, Pellicano E, Mojzisch A, Krug K. Developmental Trajectory of Social Influence Integration Into Perceptual Decisions in Children. Proc Natl Acad Sci USA.. January 28, 2019. [Epub ahead of print]
Overactive Neurons May Explain Why SSRIs Don’t Always Work
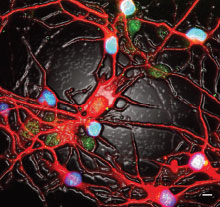
By creating neurons from patient skin samples, researchers at the Salk Institute in San Diego and colleagues have discovered a possible mechanism of antidepressant resistance. Their findings, published in Molecular Psychiatry, suggest that in some patients, neurons might become too excited by the serotonin-boosting properties of antidepressants.
The researchers studied a group of 803 patients with major depressive disorder who were treated for eight weeks with the selective serotonin reuptake inhibitors (SSRIs) citalopram or escitalopram. From this group, they selected three patients who achieved complete remission of their depression symptoms with the SSRIs (SSRI responders) by eight weeks and three patients who did not experience symptom improvements (SSRI nonresponders) for further analysis.
The researchers isolated skin cells from these patients and used cell reprogramming techniques to convert the cells into stem cells and later mature neurons. The researchers then exposed the reprogrammed neurons to serotonin to mimic the effects of taking an antidepressant like citalopram.
In the presence of serotonin, neurons derived from the SSRI nonresponders had significantly higher activity on average compared with the neurons of healthy individuals or SSRI responders, the researchers reported. Further analysis showed the hyperactivity was due to overexpression of two classes of serotonin receptors, 5-HT2A and 5-HT7. When the researchers blocked these two receptors, the neurons from nonresponders were no longer hyperactive in the presence of serotonin.
Vadodaria KC, Ji Y, Skime M, et al. Serotonin-Induced Hyperactivity in SSRI-Resistant Major Depressive Disorder Patient-Derived Neurons. Mol Psychiatry.. January 30, 2019. [Epub ahead of print]
SSRIs Best Option for Pediatric Anxiety, Meta-Analysis Finds

Selective serotonin reuptake inhibitors (SSRIs) may be the most effective treatment for patients with pediatric anxiety disorders, suggests a meta-analysis in the Journal of Clinical Psychiatry.
Researchers from the University of Cincinnati and Yale University compiled data from 22 randomized, controlled trials, including 2,623 participants. These trials included evaluations of established medications such as SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants, and benzodiazepines; there were also studies of other agents including the alpha-2 agonist guanfacine and serotonin 1A receptor agonist buspirone.
Among the tested medications, SSRIs, SNRIs, and buspirone were all superior to placebo in achieving treatment response (at least a 50 percent reduction in symptoms), with SSRIs having the strongest effect. SSRIs were also most effective when considering overall reduction in anxiety symptoms, regardless of the response rate.
The analysis also found that SNRIs had the lowest rate of treatment discontinuation due to adverse side effects, while guanfacine had the highest rate. However, there were no significant differences between the medications in relation to treatment discontinuation for any reason.
“These findings confirm recommendations from the American Academy of Child and Adolescent Psychiatry and others regarding SSRIs as first-line pharmacotherapy for pediatric anxiety disorders,” the authors wrote.
Dobson ET, Bloch MH, Strawn JR. Efficacy and Tolerability of Pharmacotherapy for Pediatric Anxiety Disorders: A Network Meta-Analysis. J Clin Psychiatry. 2019; 80(1):17r12064.
Physical Problems May Link Concussion, Depression

A history of football-related concussions is more likely to lead to depression in former NFL players who also have physical problems such as body pain, headaches, and dizziness, according to a study conducted by researchers at the Vanderbilt Sports Concussion Center and colleagues.
The investigators assessed data from 43 retired NFL players who had received comprehensive neuropsychological exams as part of a large neurological study. The exams included the Beck Depression Inventory II (BDI-II) to screen for depression and the Patient Health Questionnaire-15 (PHQ-15) to screen for somatic symptoms.
Twenty-nine of the 43 former players reported minimal depressive symptoms, nine reported symptoms of mild depression (BDI-II score of 14 to 19), three reported symptoms of moderate depression (BDI-II score of 20 to 28), and two reported symptoms of severe depression (BDI-II score of 29 to 63).
There was no connection between concussion history and depressive symptoms in the players whose PHQ-15 scores were below the study average of 5.35. In contrast, former players with PHQ-15 scores at or above the average exhibited more severe depression symptoms if they had more concussions. The researchers calculated that the presence of somatic symptoms contributed about twice as much to an individual’s depression as the concussions.
“If a retired athlete reports an extensive history of SRC [sport-related concussion] and somatic or depressive symptomatology, referral to a sports psychiatrist or clinical neuropsychologist is recommended for further assessment … and to differentiate depressive symptoms as purely somatic, psychiatric, or mixed,” the authors wrote.
This study was published in the Journal of Neuropsychiatry and Clinical Neurosciences.
Brett BL, Mummareddy N, Kuhn AW, et al. The Relationship Between Prior Concussions and Depression Is Modified by Somatic Symptomatology in Retired NFL Athletes. J Neuropsychiatry Clin Neurosci. 2019; 31(1): 17-24.
Yeast Infection Impairs Memory in Mice

A study published in Nature Communications reports that the infectious yeast Candida albicans can cross the blood-brain barrier and impair memory in mice. This suggests that fungal infections may be a risk factor for dementia.
Researchers at Baylor College of Medicine and colleagues injected mice with low levels of Candida. The injected mice showed no physical problems or stress and cleared out the infectious yeast in about 10 days. However, during this time, mice infected with Candida did show worse working memory compared with control mice as measured by maze tests. Once the infection cleared, the mice performed better.
The researchers observed that the yeast entered the brain and induced cerebritis (the formation of small inflammatory lesions). The researchers termed these lesions fungal-induced glial granulomas, or FIGGs. The FIGGs contained numerous inflammatory molecules, including amyloid beta fragments, which were involved in helping clear the yeast from the brain.
Although the memory problems were transient in this study, the authors suggested that repeated low-grade fungal infections and resulting cerebritis over many years might contribute to lasting cognitive defects. ■
Wu Y, Du S, Johnson JL, et al. Microglia and Amyloid Precursor Protein Coordinate Control of Transient Candida Cerebritis With Memory Deficits? Nat Commun. 2019;10(1): 58.



