Journal Digest
Low-Cost Virtual Reality Intervention Benefits Patients With Acrophobia

A rudimentary virtual reality (VR) intervention that uses $10 cardboard goggles, a smartphone, and self-guided cognitive-behavioral therapy (CBT) via a mobile app can reduce symptoms of acrophobia (fear of heights), according to a study published in JAMA Psychiatry.
Researchers at Vrije Universiteit in Amsterdam and colleagues assigned 193 adults with acrophobia to receive either the self-guided VR treatment, known as ZeroPhobia, or be placed on a wait list. ZeroPhobia, which includes six animated, game-like modules that incorporate CBT principles and techniques, was downloaded onto the smartphones of the participants; the low-cost goggles were provided to simulate the VR effect. Participants were asked to complete all six modules within three weeks in an environment of their choosing.
After three weeks, anxiety scores (measured on the Acrophobia Questionnaire–Anxiety scale) dropped from an average of 68.62 at baseline to 39.55 in the ZeroPhobia group, compared with a drop from 67.91 to 60.41 in the wait-list group. The reductions in acrophobia symptoms were maintained at a follow-up assessment three months later. Aside from some transient cases of cyber sickness (headaches and dizziness), the participants found the VR intervention to be tolerable and user friendly.
“One of the key strengths of the present study was its ecological validity because the intervention was conducted in the participants’ natural environments instead of a research laboratory,” the authors wrote. “Furthermore, participants received no guidance when using the VR-CBT app or filling in assessments, thereby ruling out any influence of human contact.”
Donker T, Cornelisz I, van Klaveren C, et al. Effectiveness of Self-Guided App-Based Virtual Reality Cognitive-Behavior Therapy for Acrophobia: A Randomized Clinical Trial. JAMA Psychiatry. March 20, 2019. [Epub ahead of print]
Blood Pressure, Lipid Drugs Don’t Slow Cognitive Decline

Long-term treatment with blood pressure and/or lipid-lowering medications does not seem to slow cognitive decline, according to findings from the multinational Heart Outcomes Prevention Evaluation-3 (HOPE-3) study.
More than 12,000 men (age 55 and over) and women (age 60 and over) with no known cardiovascular disease (CVD) were enrolled in the HOPE-3 study. The participants were assigned to receive either the hypertensive medications candesartan plus hydrochlorothiazide, the cholesterol drug rosuvastatin, both, or neither. The primary aim of HOPE-3 was to see if these preventive medications lowered the risk of CVD, but participants age 70 or older at baseline were also asked to take periodic cognitive tests to see if these medications might preserve memory.
Based on an analysis of cognitive data from 2,361 participants, who were followed for about 5.7 years, the investigators found no differences in cognitive decline over the years among any of the four groups. However, an exploratory analysis of study participants who had the highest blood pressure and lipid levels at baseline (average systolic blood pressure of 156.3 mm Hg and low-density lipoprotein of 164.7 mg/dL) found that the combination treatment may slow the rate of cognitive decline.
In addition, the investigators found no evidence that long-term statin use worsens cognition, which has been suggested by some previous research. These findings were published in Neurology.
Bosch J, O’Donnell M, Swaminathan B, et al. Effects of Blood Pressure and Lipid Lowering on Cognition: Results From the HOPE-3 Study. Neurology. 2019; 92(13): e1435-e1446.
Retinal Blood Vessel Scans May Reveal Alzheimer’s
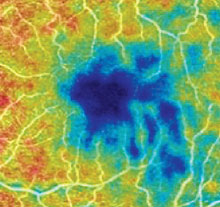
A study conducted by investigators at Duke University Eye Center suggests that a loss of blood vessels in the retina could be a biomarker of Alzheimer’s disease. The study was published in Ophthalmology Retina.
The investigators conducted high-resolution retinal scans of 39 adults with Alzheimer’s, 37 with mild cognitive impairment (MCI), and 133 control participants with no cognitive problems. The researchers used a noninvasive technique known as optical coherence tomography angiography (OCTA) to measure the density of the tiny blood vessels at the back of the eye.
The scans revealed that people with Alzheimer’s had significantly fewer retinal blood vessels compared with controls and people with MCI, even after adjusting for factors such as age, sex, and education. There were no significant differences between controls and people with MCI, which suggests this loss in blood vessel density may be specific to Alzheimer’s.
“It’s possible that these changes in blood vessel density in the retina could mirror what’s going on in the tiny blood vessels in the brain, perhaps before we are able to detect any changes in cognition,” said lead study author Sharon Fekrat, M.D., in a press release.
Yoon SP, Grewal DS, Thompson AC, et al. Retinal Microvascular and Neurodegenerative Changes in Alzheimer’s Disease and Mild Cognitive Impairment Compared with Control Participants. Ophthalmology Retina. March 11, 2019. [Epub ahead of print]
Genetic Analysis Uncovers Over 400 Schizophrenia-Associated Genetic Variants

Conducting a comprehensive analysis of DNA from more than 40,000 people with schizophrenia and 65,000 controls, researchers at Icahn School of Medicine at Mount Sinai have identified 413 genetic variants associated with schizophrenia as well as the brain regions where these variants may exert their effects.
According to the study, which was published in Nature Genetics, the 413 variants identified are associated with 256 different genes and 36 molecular pathways. The study revealed a genetic connection between schizophrenia and hexosaminidase A (HEX-A) deficiency. HEX-A is a protein that helps prevent the buildup of toxic molecules in cell’s recycling centers, or lysosomes; a complete loss of HEX-A leads to Tay-Sachs disease.
The study also revealed a connection between schizophrenia and porphyrins, chemicals that help hemoglobin function properly. People with porphyric disorders present with both metabolic and behavioral symptoms and may have contributed to the illnesses that affected Vincent van Gogh and King George III, the authors noted.
The researchers also analyzed gene expression data. Abnormal gene expression due to the identified variants was found in 13 brain regions across the lifespan; many of the genes were turned on during pregnancy but others were not active until adolescence or adulthood. ■
Huckins LM, Dobbyn A, Ruderfer DM, et al. Gene Expression Imputation Across Multiple Brain Regions Provides Insights Into Schizophrenia Risk. Nat Genet. March 25, 2019. [Epub ahead of print]



