‘Black Men in Psychiatry Early Pipeline Program’ Highlights Mentoring, Relationship Building
Abstract
Speakers at the Black Psychiatrists of America’s spring conference shared their experiences as mentors and students in the program.
According to an Association of American Medical Colleges (AAMC) 2015 report, the number of black men matriculating into medical school has decreased 5% since 1978. A fact sheet by AAMC also notes that black men comprise only 1.5% of total U.S. practicing psychiatrists and 2.6% of male U.S. practicing psychiatrists. APA’s Black Men in Psychiatry Early Pipeline Program (BMEPP), part of APA’s Workforce Inclusion Pipeline Program, seeks to address this disparity by providing black male undergraduates with mentorship, assistance with preparing for the MCAT and medical school applications, and other opportunities. The program was discussed in the session “Roadblocks of Black Men in Psychiatry” at the Black Psychiatrists of America’s 50th Anniversary Psychiatry Conference and Celebration in April at National Harbor, Md.
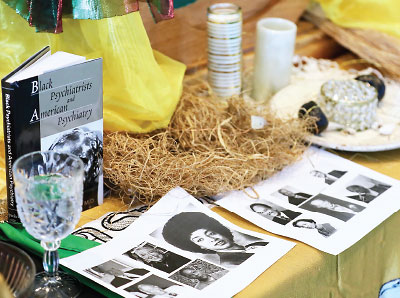
On display at the meeting of the Black Psychiatrists of America was a memorial honoring prominent black psychiatrists and commemorating black history.
“Barriers to black men entering medicine may be attributed to a lack of mentorship and role models, the quality of education [they’ve received], the cost of education, and the public perception of black men,” said Vabren Watts, Ph.D., deputy director of APA’s Division of Diversity and Health Equity (DDHE), in the session’s first presentation. “The program’s objectives are to address workforce disparities by exposing black men to the field of psychiatry and to reduce mental health disparities through education about stigma, early intervention, and prevention of mental health issues within underserved black communities.”
In an interview with Psychiatric News after the meeting, Watts explained the impetus for the program.
“Research shows that diversity in the physician workforce leads to improved access to health care for racial and ethnic minorities because minority physicians are significantly more likely than nonminorities to serve in minority and medically underserved communities,” Watts said. “This is relevant across all medical specialties, including psychiatry. Building a pipeline for more black males to enter psychiatry and work with underserved communities falls in line with the APA strategic initiative of eradicating mental health disparities for historically marginalized populations.”
Each BMEPP participant is paired with a mentor psychiatrist like Steven Starks, M.D., a geriatric psychiatrist and a Health and Aging Policy Fellow. In his presentation, Starks reflected on his experience in medical school and why he became a BMEPP mentor.
“I wasn’t offered opportunities to which other people were granted access or able to connect to networks others were,” said Starks, adding that he had to create his own coalitions and networks.
Starks, who is also an American Political Science Association Congressional Fellow who works in the Office of the Speaker of the U.S. House of Representatives, encourages black male students to be proactive, forge as many supportive relationships as possible, and not to listen to naysayers.
“Don’t let the odds intimidate you. It can be overwhelming when you think that only 6% of medical school graduates are black,” Starks said. “Hold on to your dreams and goals despite how other people may feel about it.”

Norman Harris II (left), a BMEPP participant mentored by APA President Altha Stewart, M.D., will spend a year in South Africa as a Fulbright scholar before attending medical school. Behind them is Steven Starks, M.D., a geriatric psychiatrist and congressional fellow.
Norman Harris II, a recent graduate of Howard University in Washington, D.C., and a BMEPP participant, recounted the benefits of the program, including attending APA meetings and conferences.
“We became adept at networking with medical students and early- and late-career psychiatrists and gained an understanding of the importance of mental health in our society,” Harris said. “Seeing people in the field who are like me gives me the motivation to do it. If they’re doing it, why not me?”
Harris will introduce his BMEPP mentor, APA President Altha Stewart M.D., before her presidential address at the Opening Session of APA’s 2019 Annual Meeting in San Francisco. Harris will teach English in South Africa as a Fulbright Scholar for a year before going to medical school.
The other original students in the program from Howard are Emmanuel Demissie, who is being mentored by APA CEO and Medical Director Saul Levin, M.D., M.P.A.; and Rajon Scott, who is being mentored by Curley Bonds, M.D., chief deputy director of clinical operations at the Los Angeles County Department of Mental Health. ■



