Journal Digest
Researchers Identify Gene Linked With Regulation of Fear, Anxiety

Fear and anxiety may be moderated in part by a gene known as P4h-tm, according to a study in Neuropharmacology. Researchers at the University of Eastern Finland and colleagues found that mice that had this gene knocked out displayed less fear and greater social interaction compared with regular lab mice.
P4h-tm encodes the P4H-TM protein (transmembrane prolyl-4-hydroxylase), which helps cells adapt to a sudden lack of oxygen. To compare how animals with and without the P4h-tm gene react to oxygen changes in the environment, the researchers placed mice in a sealed container that was then filled with 10% carbon dioxide. Whereas control mice froze in place in response to the change in oxygen levels, the mice without the P4h-tm gene did not exhibit this freeze response. Additional tests revealed that P4h-tm knockout mice showed greater social interaction and fewer fear responses than control mice.
An analysis of brain tissue in control mice showed that P4H-TM was highly expressed in the amygdala—the brain’s center for emotion regulation. This further supports this protein’s role in regulating fear and social anxiety.
“The courageousness and perseverance observed in P4h-tm [knockout] mice are behavioral characteristics that are often the desired outcomes of psychiatric therapy,” the authors wrote. “This raises the intriguing idea of targeting P4H-TM with selective pharmacotherapy for treatment of anxiety and depression.”
Leinonen H, Koivisto H, Lipponen HR, et al. Null Mutation in P4h-tm Leads to Decreased Fear and Anxiety and Increased Social Behavior in Mice. Neuropharmacology. April 25, 2019. [Epub ahead of print]
Massive Genetic Analysis Uncovers 20 Risk Variants for Bipolar Disorder
In the largest genetic analysis of patients with bipolar disorder to date, a multinational research team has identified 20 new genetic variants that appear to increase the risk of bipolar disorder. The findings were published in Nature Genetics.
The group, led by investigators at Icahn School of Medicine at Mount Sinai, analyzed DNA samples from 20,352 patients with bipolar disorder and 31,358 controls without the disorder. They identified 822 potential candidates for genetic risk who were re-tested in an independent sample of 9,412 bipolar patients and 137,760 controls.
A total of 30 genetic risk variants were identified in these combined samples, of which 20 were previously unidentified in bipolar disorder studies. However, eight of these 20 novel bipolar risk variants had been previously linked with increased risk of schizophrenia.
These 20 novel variants were associated with genes involved in numerous biological processes, including insulin regulation and endocannabinoid signaling.
The investigators next compared DNA samples of people with bipolar I disorder and bipolar II disorder. They found that most of the variants associated with both bipolar disorder and schizophrenia were primarily related to bipolar I disorder; genetic variants prominent in bipolar II disorder were more strongly correlated with major depressive disorder. The authors stated these findings support the idea that these two bipolar subtypes should be considered distinct conditions.
Stahl EA, Breen G, Forstner AJ, et al. Genome-Wide Association Study Identifies 30 Loci Associated With Bipolar Disorder. Nat Genet.. May 1, 2019. [Epub ahead of print]
Depression, Anger Problems May Not Be Good Criteria for CTE Diagnosis

Some health professionals have proposed that anger control problems and depression should be defining clinical features of chronic traumatic encephalopathy (CTE), a neurodegenerative condition brought on by head trauma. A study appearing in the Journal of Neuropsychiatry and Clinical Neurosciences shows that there is a high prevalence of hostility and depression among middle-aged men without CTE, which should be considered when thinking about a CTE diagnosis.
Researchers at Harvard Medical School and colleagues assessed data from 166 men aged 40 to 60 with no history of head injury who completed a National Institutes of Health survey on neurological and behavioral function. They found that 17.5% of the participants scored positive on at least one of the five questions related to physical aggression, with 11.4% reporting they may hit someone if provoked. Additionally, 21.1% of respondents reported some recent anger, 25.9% reported recent depression, and 26.5% reported recent irritation.
The researchers found a strong correlation between anger and depression traits; participants who reported some degree of depression, anxiety, anger, or hostility were more likely to experience one or more of the other behaviors as well.
“It is important for clinicians and researchers to appreciate that when irritability and anger control problems emerge or clearly worsen over time, these problems might be associated with life stress, marital problems, sleep disturbance, chronic pain, chronic headaches, substance abuse, depression, a neurological problem, a neurodegenerative disease, or a combination of factors,” the authors wrote.
Iverson GL, Terry DP, Luz M, et al. Anger and Depression in Middle-Aged Men: Implications for a Clinical Diagnosis of Chronic Traumatic Encephalopathy. J Neuropsychiatry Clin Neurosci. April 25, 2019. [Epub ahead of print]
Genomic Analysis Identifies Specific Neural Cells Affected by Autism
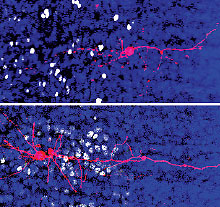
A team led by researchers at the University of California, San Francisco, has identified cell-specific genetic changes associated with symptom severity in people with autism spectrum disorder (ASD).
As reported in Science, the researchers used an approach termed single-cell genomics to analyze brain tissue from 15 patients with ASD and 16 matched controls. They generated gene expression profiles of over 52,000 cells (representing 17 cell types) from each of the two groups. Since seizures are a common neurologic complication in patients with ASD, the researchers also analyzed gene expression from seven patients with epilepsy but no ASD as a further control.
Analysis of this comprehensive genetic database revealed that the biological pathways that regulate the function of existing neuronal connections (synapses) as well as those that regulate the growth of new connections are highly affected in ASD. Specifically, a set of gene expression changes in cortical projection neurons (the primary system of communication in and out of the frontal cortex) correlated with the severity of behavioral symptoms in patients with ASD. The researchers also identified important gene expression differences in supporting brain cells known as microglia. In both instances, the researchers confirmed that gene expression changes were due to ASD and not induced by seizures.
“The ASD-specific genes highly correlated with clinical phenotypes represent high-priority therapeutic targets for ASD,” the researchers wrote.
Velmeshev D, Schirmer L, Jung D, et al. Single-Cell Genomics Identifies Cell Type–Specific Molecular Changes in Autism. Science. May 17, 2019. [Epub ahead of print]
Stressful Physician Training Affects Telomere Attrition

The long and rigorous schedules of first-year medical residents lead to a dramatic shortening of a cell’s telomeres (the caps at the ends of chromosomes that keep DNA stable). Telomere length is considered a biological marker of stress, and short telomeres are associated with numerous physical and mental health problems.
This finding comes from a study published in Biological Psychiatry.
Investigators at Kaiser Permanente and colleagues enrolled 250 first-year residents across 55 U.S. medical institutions for this study. All participants provided saliva for DNA analysis at the start and end of their training year and completed online surveys every three months that assessed various demographic and psychological measures.
The investigators found that the residents experienced an average telomere reduction of 143.5 base pairs over the year. This was almost six times as much telomere attrition as has been reported for the general population (~25 base pairs/year). Greater telomere reduction was associated with longer hours worked.
“A large and growing body of work has identified that physician training and practice adversely affect a range [of] mental health outcomes, including burnout, depression, and suicide risk,” the investigators wrote. “These are the first data showing a link between the subjectively stressful experience of physician training and an objective marker of cellular stress exposure.”
Ridout KK, Ridout SJ, Guille C, et al. Physician Training Stress and Accelerated Cellular Aging. Biol Psychiatry. May 9, 2019. [Epub ahead of print]
Living Alone Increases Risk of Mental Illness

Living alone, regardless of age, increases the risk of common mental disorders, such as depression and anxiety, according to a new report appearing in PLoS One. Previous research has established a link between living alone and mental disorders, but most studies have focused on older adults and depression.
Investigators at the University of Barcelona in Spain and Versailles University in France analyzed data from the 1993, 2000, and 2007 editions of the National Psychiatric Morbidity Survey, a community-based survey on mental health conducted by the United Kingdom every seven years.
They found that the prevalence of common mental disorders (defined in the survey as depression, generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, or a phobia) was higher in individuals living alone than in those not living alone in all three survey years. The association between living alone and risk of common mental disorders remained about the same between 1993 and 2007, ranging from 1.39 to 2.43 times higher odds for common mental disorders in people living alone compared with those not living alone. The association between living alone and common mental disorders was observed in all age groups including young adults and both sexes.
Additional analysis revealed that overall feelings of loneliness explained 84% of the association between living alone and common mental disorders, the authors reported.
“Interventions addressing loneliness among individuals living alone may be particularly important for the mental wellbeing of this vulnerable population,” the authors wrote. ■
Jacob L, Haro JM, Koyanagi A. Relationship Between Living Alone and Common Mental Disorders in the 1993, 2000, and 2007 National Psychiatric Morbidity Surveys. PLoS ONE. 2019; 14(5): e0215182.



