AMA Backs Alignment of Regs Governing SUD Treatment Records With HIPAA
Abstract
The resolution on 42 CFR Part 2 was one of two put forward by the Section Council on Psychiatry that were ultimately approved by the House. The other calls for CMS to discontinue the use of psychotropic medication as a factor contributing to Nursing Home Compare rankings.
The AMA House of Delegates voted to support the alignment of federal regulations governing the privacy of substance use disorder (SUD) records with the Health Insurance Portability and Accountability Act (HIPAA) for the purposes of treatment, payment, and health care operations.
A resolution passed by the House of Delegates last month asks the AMA to support the alignment “while maintaining protections against the use of information in criminal justice proceedings.” Such an alignment would significantly enhance the coordination of care for patients with substance use disorders or a history of substance use treatment.
More than 70% of delegates in the 500-plus-member House voted in favor of the resolution, which was sponsored by the Section Council on Psychiatry and the American Society of Addiction Medicine with support from a broad coalition of individual physicians, state delegations, and specialty societies. These included the American College of Physicians, Congress of Neurological Surgeons, and the American Clinical Neurophysiology Society. The vote occurred during last month’s Annual Meeting of the House of Delegates in Chicago.

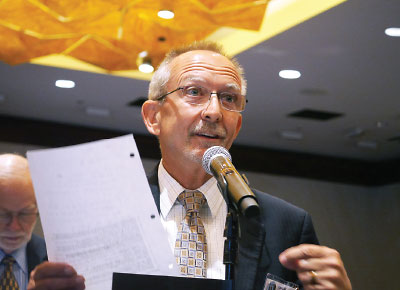
Ken Certa, M.D., tells the House of Delegates that the 42 CFR Part 2 regulations, originally intended to protect patient confidentiality, now impede coordinated care of patients with substance use disorders.
A major victory for APA delegates, the resolution calls for the AMA to support the alignment of regulations known as 42 CFR Part 2 with HIPAA. The 42 CFR Part 2 regulations, formulated in the 1970s, restrict the sharing of medical records related to substance use treatment. The regulations were originally intended to protect patient confidentiality, but they make it difficult for physicians to know whether a patient is being treated for or has a history of substance use disorder.
David Fassler, M.D., a delegate from the American Academy of Child and Adolescent Psychiatry, testified to the House that 42 CFR Part 2 “jeopardizes patient safety, undermines collaborative care, and further stigmatizes substance use disorders.” Other physicians made similar remarks.
“What is most heartening about the passage of our resolution is the great support from other parts of the AMA,” Section Council member Ken Certa, M.D., told Psychiatric News. “Testimony from delegates from Utah, Colorado, and Illinois demonstrated the widespread desire for the end to stigmatization of substance use disorder treatment. There is a recognition that the outdated federal rules that mandate a separate chart for addiction treatment lead to incomplete information, which puts lives at risk.”
“Patients should be able to protect their personal health information, and patient permission for information sharing should be obtained,” addiction psychiatrist Michael Miller, M.D., a delegate from Wisconsin, said after the meeting. “But once it is obtained, information among health care professionals should be bidirectional and unimpeded by outdated regulations that were created many years before electronic health records or health information exchanges existed and before the emerging trends in collaborative care and the integration of behavioral health care into general medical settings.”
Psychotropics Appropriate in Long-Term Care
Also an important victory for the Section Council on Psychiatry was the unanimous adoption by the House of a resolution on access to psychiatric treatment in long-term care settings. The resolution, sponsored by APA and the American Association for Geriatric Psychiatry (AAGP), asks the Centers for Medicare and Medicaid Services (CMS) to acknowledge that psychotropic medications can be an appropriate long-term-care treatment for patients with chronic mental illness. Importantly, the resolution seeks to have CMS stop including measures regarding use of antipsychotics at a facility in its Nursing Home Compare rankings, unless the data utilized are limited to medically inappropriate administration of these medications. Currently Nursing Home Compare reports the percent of residents who received an antipsychotic medication and the percent of residents who newly received an antipsychotic medication.
Geriatric psychiatrist Allan Anderson, M.D., says some long-term-care facilities will not accept patients being treated with antipsychotics.
“An estimated one-third to one-half of nursing home residents suffer from mental illness, including dementia,” said Sandra Swantek, M.D., a delegate from AAGP, in testimony. For many of these patients use of an antipsychotic under carefully monitored circumstances is medically justified.
Swantek told delegates that long-term care facilities attempt to get the highest possible rating, which often results in mandated taper and discontinuation of antipsychotic medications, regardless of psychiatric diagnosis.
“APA and the AAGP recently conducted a survey of member mental health clinicians caring for older adults in long-term-care settings,” Swantek said. “Over 80% of respondents reported requests to alter prescribing practices so that the facility could achieve a higher quality rating. Over 80% of the clinicians also reported that patients were destabilized because of the mandated taper. In a number of cases, hospitalizations resulted with some clinicians reporting difficulty readmitting the patient to the long-term-care facility.”
Section council member Paul O’Leary, M.D., said, “Old age is not a cure for mental illness, yet individuals needing long-term care are being tapered off of their medications because of a blanket policy that doesn’t take into account the needs of the patient.” ■
The reports and resolutions approved by the House of Delegates are posted here.



