SUD Patients More Susceptible to COVID-19, Adverse Outcomes
Abstract
Although individuals with substance use disorders made up only 10.3% of the 73 million patients involved in a recent study, they represented 15.6% of COVID-19 cases. Policy changes and effective interventions are needed now to help this population.
Engaging in exercise, getting a good night’s sleep, and limiting alcohol consumption have long been recognized as preventive strategies to reduce the onset of depression. Now, a study in AJP in Advance suggests that the most impactful activity a person can do to prevent depression is to confide in others.

Patients with SUDs may be reluctant to seek health care for fear of being mistreated due to stigma and discrimination, says Nora Volkow, M.D.
For the past two decades, the United States has been in the grips of an opioid crisis that, despite interventions, has not slowed down. “Now, amid the opioid crisis, comes the COVID pandemic,” Nora Volkow, M.D., director of the National Institute on Drug Abuse (NIDA), told Psychiatric News. “When you have two crises colliding with one another, it can result in very devastating consequences.”
According to a study that Volkow and her colleagues published in Molecular Psychiatry on September 14, people with SUDs are more susceptible to COVID-19 and its complications. The association was especially pronounced for individuals with opioid use disorder (OUD), followed by tobacco use disorder (TUD).
The researchers analyzed electronic health record data collected by IBM Watson Health Explorys from 360 hospitals across the United States from 1999 until June 15, 2020. The data included information from more than 73 million unique patients, 7.5 million of whom were diagnosed with an SUD. The disorder types included OUD, TUD, alcohol use disorder (AUD), cannabis use disorder, and cocaine use disorder. Of this population, more than 12,000 patients were diagnosed with COVID-19, and 1,880 were diagnosed with both an SUD and COVID-19.
Patients with recent OUD diagnoses (meaning they had been diagnosed within the past year) had the highest risk of COVID-19 of any other SUD type and were eight times more likely to develop COVID-19 than those without an SUD diagnosis. Patients with SUDs who developed COVID-19 also had significantly worse outcomes compared with patients without SUDs, with higher rates of hospitalization and death.
The researchers were not surprised by their findings, said Rong Xu, Ph.D., a study co-author and director and professor at the Center for Artificial Intelligence in Drug Discovery at Case Western Reserve University. “Our study needs to be replicated in other populations, but I don’t think we need to wait until that point before we start creating policy changes or paying special attention to this especially vulnerable population,” she said.
The authors noted some study limitations, including the limited number of individuals who have been tested for COVID-19; the use of electronic health record data that may reflect under- , over- , or misdiagnoses; and the potential underreporting of people with SUDs because of their difficulty in accessing health care.
People with SUDs often have comorbid medical conditions, Volkow explained, such as cardiovascular diseases, that may put them at higher risk for COVID-19. But just as significant as the medical comorbidities are social factors among this population that increase risk, she added. People with SUDs are more likely to come from a low socioeconomic background, be incarcerated, and experience homelessness. Also, they are much less likely to have access to quality health care.
“Then you have the issue of stigma and discrimination against people with addiction in our country,” Volkow said. “Patients may be reluctant to seek care because they don’t want to be mistreated.”
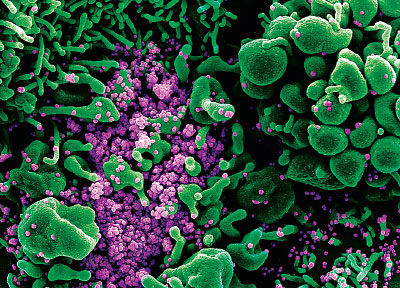
Colorized scanning electron micrograph of a cell (green) heavily infected with SARS-COV-2 virus particles (purple) from a patient sample.
“This is probably the largest set of data that show us what a substance use disorder diagnosis means in terms of COVID-19 risk and outcomes,” said Smita Das, M.D., Ph.D., M.P.H., a clinical assistant professor of psychiatry and behavioral health sciences at Stanford University School of Medicine and a member of APA’s Council on Addiction Psychiatry.
The racial disparities that the pandemic has already exposed were similarly evident among patients with SUDs in the study. Among those with recent SUD diagnoses, African Americans had a significantly higher risk of developing COVID-19 than their White counterparts, as well as a higher risk for worse outcomes, including hospitalization and death.
“The impacts of racial injustice in our country are undeniable, and we can’t ignore them,” Das said. “Ultimately, the report highlights something that we’ve known about for a long time and that we’ve struggled with as a country. But by adding the context of COVID-19, my hope is that more people will finally pay attention.”
The pandemic has the potential to worsen the already devastating opioid crisis, Volkow said. Mental health professionals often encourage people with SUDs to avoid stressful situations. “But how do we avoid COVID-19?” she said. “We’ve seen reports from people all over the country: People are relapsing.” So, too, are overdoses increasing across the country, Volkow pointed out (see Psychiatric News).
Das also worries that people are turning to extremely toxic drugs, such as fentanyl and methamphetamine, because of supply chain disruptions caused by the pandemic. So, too, is she concerned that people are more likely to inject drugs alone due to social distancing measures, reducing the likelihood that someone else can intervene if an overdose occurs.
Das noted that the United States has been experiencing major public health crises related to multiple SUDs. There are thousands of deaths every year caused by opioid overdoses, as well as diseases caused by tobacco use. “We know people with SUDs often don’t have access to the treatments that they need,” she said. “During the pandemic, there have been multiple shifts that have, in some ways, limited access, but I’m hopeful that over time access will expand.”
Health systems have had to focus on delivering the most essential services necessary to patients, and unfortunately in some cases treatment for people with SUDs has been pushed to the side, she said. Nonetheless some clinics are finding ways to broaden access to care during the pandemic.
“In my clinic, I treat people with tobacco use disorder, and it’s been nice in some ways because people who live in remote parts of California and couldn’t drive to the clinic are able to see me through telemedicine,” she said. “I’ve also noticed that some are more motivated to quit smoking because of the pandemic. I think some people are able to engage more right now, despite the circumstances.”
The study was funded by the National Institute on Drug Abuse, the Eunice Kennedy Shriver National Institute for Child Health and Human Development, the National Institute on Aging, the American Cancer Society, and the Clinical Translational Science Collaborative of Cleveland. ■
“COVID-19 Risk and Outcomes in Patients With Substance Use Disorders: Analyses From Electronic Health Records in the United States” is posted here.



