Marijuana Use, Rates of Mental Illness Rise, Survey Finds
Abstract
With more Americans getting medication treatment, the number of people with opioid use disorders fell sharply in 2019; however, the opioid overdose death rate rose, along with mental illness and marijuana use.
Opioid use disorder (OUD) dropped nearly 24% in 2019, affecting 1.6 million Americans, down from 2.1 million the year before. The decline continues a five-year trend, according to the results of the 2019 National Survey on Drug Use and Health (NSDUH). In addition, past-year heroin use fell among young adults (18 to 25 years old).
The NSDUH is a household survey of 68,000 Americans aged 12 and older by the Substance Abuse and Mental Health Services Administration (SAMHSA). The results are used to gauge the nation’s state of substance use, mental illness, and treatment services.
“It shows that when we put resources into a major national public health problem, we can make a very positive impact,” said Elinore F. McCance-Katz, M.D., Ph.D., assistant secretary for mental health and substance use at SAMHSA, in a statement. “We need to be doing that in other circumstances that relate to behavioral health as well.”
McCance-Katz attributed the decline to wider access to medication treatment for OUD, psychosocial supports, and community recovery services. Nearly 1.5 million Americans received medication treatment in 2019, the highest number on record, up from 1.3 million the prior year.
Other measures of the opioid epidemic seemed to show mixed results. Prescription pain reliever misuse, which makes up the vast majority (97%) of opioid misuse, dropped slightly among adolescents and young adults in 2019, but remained flat in adults aged 26 and older. Meanwhile, a key metric of the opioid epidemic—opioid overdose deaths—rose 4.6%, McCance-Katz noted.
“This underscores the risks to Americans who use potent synthetic opioids such as fentanyl that continue to kill our people by the tens of thousands,” she said. “It’s very important we continue to address opioid use disorder and that we do outreach to help people who may be reticent to enter treatment on their own.”
The percentage of Americans aged 12 and older with past-month binge drinking (24%) and past-month heavy alcohol use (6%) showed little change in 2019 from the prior year, according to the report. Young adults had the highest rates of past-month binge drinking (34%) and heavy alcohol use (8%), but the rates have declined significantly in this group over the past five years.
Meanwhile, illicit drug use rose in 2019, with nearly 21% of Americans aged 12 and older reporting past-year use, led primarily by rising use of marijuana. Past-year use of marijuana reached its highest level in 10 years, with 18% reporting use and increases in the number of daily or near-daily users.
“Marijuana is not the same drug that it was a generation ago, or even a few years ago,” McCance-Katz said, citing its much higher THC content and availability in multiple product forms. “There are a lot of health concerns, yet these seem to be drowned out by a multibillion-dollar industry that tells people that marijuana is harmless.”
Marijuana intoxication is associated with motor vehicle accidents and increased risk for psychotic disorders and other substance use disorders (SUDs), she said.
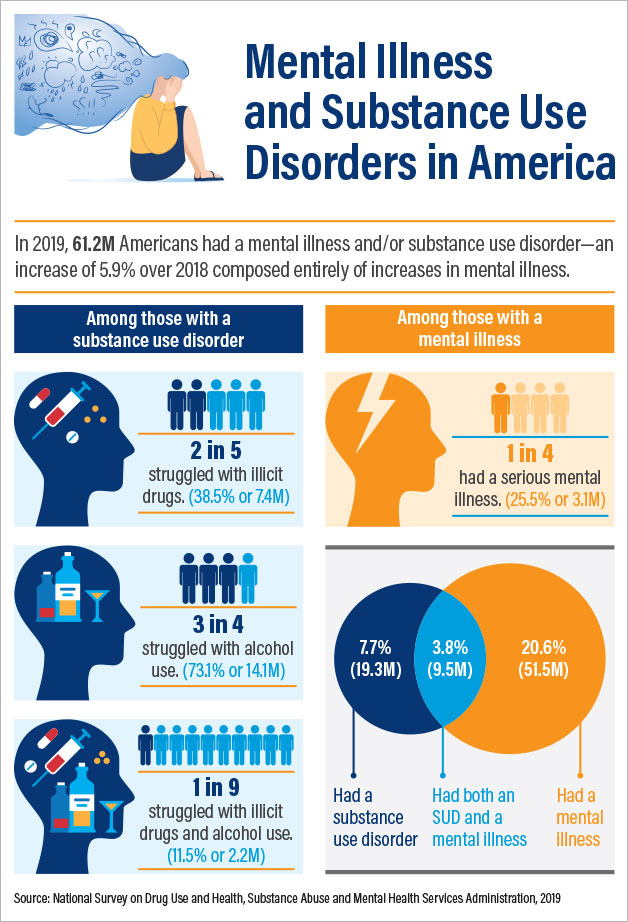
The percentage of adults with a past-year mental illness and SUD is on the rise. That’s of great concern, because the data demonstrate that substance use is associated with other mental illnesses and vice versa, McCance-Katz said. Whereas 17% of adults with no mental illness used illicit drugs in 2019, the proportion climbed to 39% among those with any mental illness. Among those with serious mental illness, nearly half (49%) used illicit drugs.
Similarly, adolescents who had a major depressive episode in 2019 were twice as likely to have used marijuana or opioids that year or to have binged on alcohol as their peers, she said. “It’s very important that when we see adolescents with major depressive disorder that we screen for and treat illicit substance use.”
About 1 in 5 adults (18 and older)—nearly 52 million—had mental illness in 2019, amounting to an 8% increase over the prior year and continuing a five-year upward trend across all age groups. The number of adults with serious mental illness also rose steeply in 2019 to 13 million, amounting to a 15% increase from the prior year.
Young adults had the highest rate of mental illness in 2019, affecting more than 29%. More than 15% of young adults had a major depressive episode, and nearly 12% had serious thoughts of suicide. More than 62% of young adults with mental illness received no mental health services.
Young adults also had nearly double the rate of past-year substance use disorder (SUD) as other adults, nearly 14%. Similarly, there was a sharp rise among adolescents (aged 12 to 17) in 2019 in the rate of major depressive episode (MDE) and MDE with severe impairment, reaching nearly 16% and 11%, respectively.
McCance-Katz noted that the NSDUH was conducted in 2019 prior to the start of the COVID-19 pandemic. “We’re already seeing the negative mental health effects of COVID ... [and] evidence of the devastation.” She noted a 10-fold increase in calls to SAMHSA’s Disaster Distress helpline as well as increases in the following: suicides and emergency department visits for suicide; reports of domestic violence, including those made to domestic violence helplines; reports of child abuse and infant deaths attributed to child abuse; and in some areas of the country, 25% to 50% increases in opioid overdose deaths, compared with the same timeframes in 2019. ■
The 2019 NSDUH report is posted here.



