Psychiatrists Can Take Steps To Protect Against Malpractice Claims
Abstract
A session at this year’s Annual Meeting will explore current professional liability issues facing psychiatrists, including those involving electronic communications and treatment of minors.
A Presidential Session at this year’s Annual Meeting will help psychiatrists better understand how to protect themselves from malpractice claims and navigate the legal process should a suit be brought against them. Fortunately, psychiatrists are less likely to be sued for malpractice than the vast majority of physicians in other specialties, especially procedural-based specialties. According to data from the National Practitioner Data Bank (NPDB), psychiatrists account for approximately 4% of all active physicians, but only for 1% of all paid medical malpractice claims in the United States.
Once sued, however, psychiatrists have to navigate a complicated and nonintuitive legal process that can lead to considerable stress. Furthermore, while rates of malpractice actions in psychiatry are relatively low compared with other specialties, psychiatrists are more likely than other specialists to be the recipient of disciplinary actions from state medical boards.
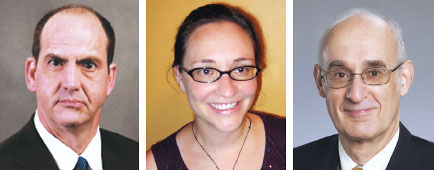
Richard Frierson, M.D., will review the common legal principles underlying malpractice lawsuits against psychiatrists, the lengthy litigation process and different stages of a malpractice suit, and the common allegations of negligence that are brought against psychiatrists. Additionally, he will outline the proper response of the psychiatrist/defendant to limit a plaintiff’s chance of success.
Susan Hatters Friedman, M.D., will focus on boundary issues and boundary violations. She will discuss the legal implications of sexual boundary violations, including state laws that have imposed criminal penalties for therapist-patient sexual interactions. She will also discuss social media and email boundaries and provide guidance on how to manage electronic communications with patients. The use of electronic communications may prompt clinicians to consider communications as informal, but it is critical that these communications remain professional and formal. Emails that are not handled appropriately can quickly become a boundary issue as the internet provides a vehicle for possible boundary violations to come into the open and for professionalism to be challenged.
Peter Ash, M.D., will explore several legal issues that differ in the practice of child and adolescent psychiatry from treating adults. Professional liability issues in the assessment and management of adolescents at risk of harming themselves or others differ somewhat from liability issues associated with adults. High-profile school shootings have prompted greater concerns about liability associated with the treatment and management of adolescents who are threatening violence. State laws vary as to the conditions under which adolescents can consent or refuse psychiatric treatment.
In addition, the age of consent to medical treatment varies among states and should guide whether a substitute decision maker or parent should be involved in making treatment decisions. Protecting confidentiality when treating minors is also more complicated, as is deciding when it is necessary to divulge clinical information to parents. ■
“Current Issues in Psychiatric Malpractice Litigation and Professional Boundaries” will be held Tuesday, April 28.



