SMI Adviser Brings Expertise on SMI to Annual Meeting
Abstract
SMI Adviser, APA’s Clinical Support System for Serious Mental Illness (SMI), will sponsor five educational sessions featuring experts in SMI. All mental health professionals are invited to visit the Mental Health Innovation Zone in the Exhibit Hall to learn more about SMI Adviser and how it can assist you in treating this population.
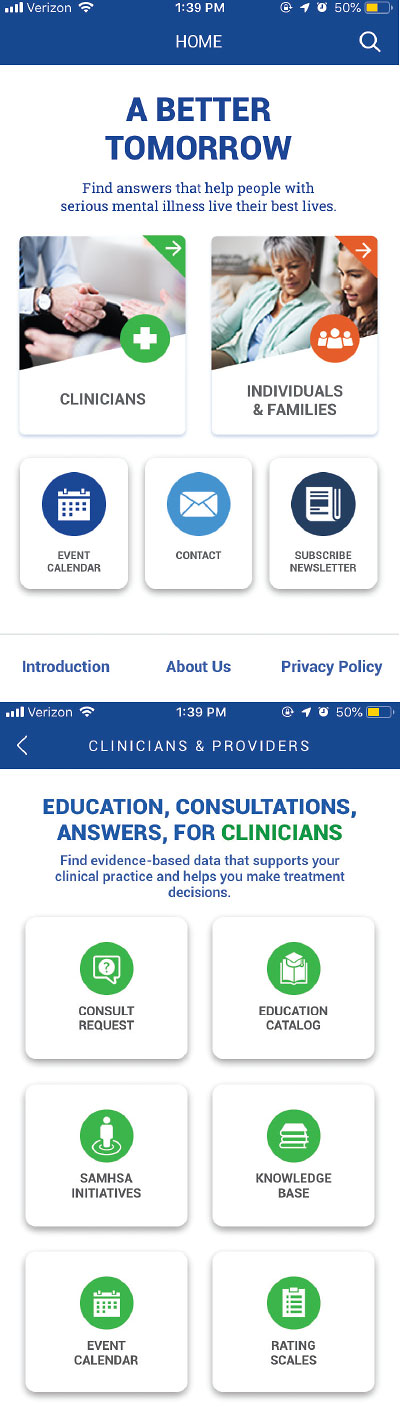
The homepage of the SMI Adviser App (top) has portals for clinicians and individuals with serious mental illness and their families. The portal for clinicians (bottom) allows them to request a free consultation and offers a large volume of resources.
Experts in serious mental illness (SMI) will present at five educational sessions sponsored by SMI Adviser, APA’s Clinical Support System for Serious Mental Illness, at this year’s Annual Meeting in Philadelphia.
Additionally, SMI experts and APA staff will be available at the SMI Adviser booth located near the Mental Health Innovation Zone in the Pennsylvania Convention Center to introduce attendees to SMI Adviser.
“This is an opportunity for all mental health professionals who work with patients with serious mental illness to learn about this exciting initiative, which is using digital technology to expand expertise in treating serious mental illness,” said APA Director of Education Tristan Gorrindo, M.D. “Using apps, consultations, and online education, we’re committed to helping all clinicians implement the best possible care when treating people with serious mental illness. We urge interested clinicians to visit us at the SMI Adviser booth and at SMI Adviser’s educational sessions to meet the SMI experts who support this initiative and to learn about how SMI Adviser is supporting front-line clinical practice.”
SMI Adivser was funded in July 2018 by a five-year, $14.2 million grant from the Substance Abuse and Mental Health Services Administration. It incorporates educational courses, fact sheets, toolkits, and consultation to expand the base of clinicians—including physicians, nurses, recovery specialists, peer-to-peer specialists, and others—able to provide evidence-based care to individuals with SMI. (SMI typically includes schizophrenia, bipolar disorder, and major depressive disorder.)
Last year, SMI Adviser expanded its reach by introducing a new app that can be downloaded for free to a smartphone (Psychiatric News). The app allows clinicians to earn educational credits, obtain consultation from experts, and access tools to support care.
Following are the educational sessions organized by SMI Adviser:
“Interview-Based Assessment of Cognitive Deficits in People With Serious Mental Illness” (Sunday, April 26, 8 a.m.-9:30 a.m.): Cognitive deficits that accompany serious mental illness are highly prevalent and can have long-term functional consequences. Enhancing treatment for these illnesses requires the implementation of cognitive assessment in routine clinical practice. Interview-based measures of cognition include the Cognitive Assessment Interview (CAI), which has been shown to be reliable, valid, and sensitive to treatment effects. This session will review the role of cognition in serious mental illness and the evidence supporting interview-based assessment. Participants will be provided with instruction on use of the CAI. Presenters include Joseph Ventura, Ph.D., and Alexander Young, M.D.
“Emerging Advances in the Use of Technology for Peer Support in SMI” (Sunday, April 26, 1 p.m.-2:30 p.m.): Peer support is an evidence-based service that has been shown to enhance the care of SMI. One limitation, however, is that patients have sometimes been unable to find the “right match” in their geographic area. Digital technology offers a solution by allowing individuals to access peer support via chatrooms, apps, and video visits. Yet there are risks as well as benefits that must be considered including online/digital privacy, ensuring access to quality peer support, and integrating peer support into clinical care. Presenters will discuss the potential of digitally facilitated peer support and offer advice on how to select and use digital services. Presenters include Patrick Hendry, John Torrous, M.D., Benjamin Druss, M.D., M.P.H., and Teri S. Brister, Ph.D.
“Alternative Treatments for SMI: ‘How-To’ for Long-Acting Injectables” (Monday, April 27, 8 a.m.-9:30 a.m.): Participants in this Learning Lab will learn about risks and benefits of existing LAI formulations. Dosing of oral antipsychotic medications and optimal conversion to LAI formulations will be detailed, including ongoing monitoring parameters. A “skills lab” will allow participants to practice giving these injections in correct anatomical sites, considering dosing, medication formulation and re-constitution, volume of injection relative to appropriate site administration, and monitoring for side effects and effectiveness of pharmacotherapy. Jacqueline Feldman, M.D., is the presenter.
“Psychiatric Advance Directives: Establishing a Patient’s Plan for a Mental Health Crisis” (Monday, April 27, 10 a.m.-11:30 a.m.): A psychiatric advance directive (PAD) is a legal tool recognized in many states that allows a person with mental illness to specify preferences for treatment and hospitalization in advance of periods of compromised decision-making capacity. Without such information, clinicians may be left to make surrogate decisions for a patient, often through a complicated court-ordered process. There is a national effort to ensure that all patients being discharged from an inpatient psychiatric unit have a valid PAD. A new PAD smartphone app has been developed to walk an individual through the creation of a PAD. The app will be demonstrated, and attendees will have the opportunity to download it. Presenters include Tristan Gorrindo, M.D., Amy Cohen, Ph.D., Teri Brister, Ph.D., and Patrick Hendry.
“Clozapine: What’s New With Our Most Effective Antipsychotic Medication” (Wednesday, April 29, 8 a.m.-9:30 a.m.): This session will review innovations in the use of clozapine, the most effective antipsychotic medication for treatment-resistant schizophrenia. Emerging point-of-care devices for obtaining white blood cell counts and serum levels at clinical practice sites will be reviewed and compared. Updates on recent changes to the Risk Evaluation and Mitigation Strategy (REMS) program will be presented, including strategies for easing clinician and patient burden. Presenters include Deanna Kelly, Pharm.D., Alexander Young, M.D., Donna Rolin, Ph.D., Jonathan M. Meyer, M.D., and Dan Cohen, M.D., Ph.D. ■



