Journal Digest: BDP, Antipsychotic, Chronic Fatigue Syndrome in Youth, Cannabis, TBI, Social Deprivation During Infancy
Hormone Fluctuations May Exacerbate Mood Changes in Women With BPD

Hormonal changes during the menstrual cycle may affect the type of aggression women with borderline personality disorder (BPD) are likely to exhibit, according to a study by researchers at the University of North Carolina. The researchers analyzed data from 15 unmedicated, naturally cycling women with BPD, who completed a mood questionnaire and ovulation test daily for 35 days.
Women displayed reactive aggression (impulsive and unplanned outbursts) most often during the luteal phase—the time after ovulation and before the start of menstruation. Proactive aggression (premeditated outbursts) were most common during the follicular phase—right after menstruation, when estrogen levels begin to rise. Overall levels of irritability were low during the follicular phase and ovulation, then began to rise during the luteal phase and peak during menstruation.
“It is possible that reactive aggression reflects an immediate impulsive response to the initially heightened irritability,” the authors wrote. “Cycling individuals with BPD attempting to reduce aggressive behavior may benefit from cycle tracking to increase awareness of these effects and to develop appropriate strategies.”
This study was published in Aggressive Behavior.
Peters JR, Owens SA, Schmalenberger KM, Eisenlohr-Moul TA. Differential Effects of the Menstrual Cycle on Reactive and Proactive Aggression in Borderline Personality Disorder. Aggress Behav. January 20, 2020. [Epub ahead of print]
Nursing Homes Vary in Off-Label Antipsychotic Use

Nursing homes that have a high proportion of residents receiving Medicaid have higher rates of inappropriate antipsychotic use, reports a study published in the Journal of the American Geriatrics Society. Inappropriate antipsychotic use reflects off-label use of these medications to treat dementia symptoms like agitation, as opposed to their indicated use to treat symptoms of psychosis.
“As the [nursing home] population continues to become more diverse, it is essential to understand mechanisms that may mitigate or enable disparities in long-term care across facilities,” the study authors wrote.
The researchers, led by a team at Brown University, evaluated data from nearly 13,000 Medicare- and Medicaid-certified nursing homes available via the Centers for Medicare and Medicaid Services’ annual nursing home surveys. They looked at the number of residents given an antipsychotic in the absence of a bipolar or schizophrenia diagnosis between 2000 and 2015.
Across all years, 19.2% of nursing home residents received antipsychotics inappropriately. Average rates of inappropriate antipsychotic use rose from 2000 to 2006, then began dropping, reaching a low of 12.7% of nursing home residents in 2015. Inappropriate use was higher among facilities in which at least 85% of residents were on Medicaid compared with facilities with fewer Medicaid recipients.
Though some previous reports have suggested racial disparities in inappropriate antipsychotic use, the researchers identified no evidence of more inappropriate use at facilities with a high proportion of black residents (36% or more) compared with those with a low proportion of black residents (less than 36%).
Fashaw S, Chisholm L, Mor V, et al. Inappropriate Antipsychotic Use: The Impact of Nursing Home Socioeconomic and Racial Composition. J Am Geriatr Soc. January 22, 2020. [Epub ahead of print]
Chronic Fatigue Syndrome Often Goes Undiagnosed in Youth

While rare, most youth with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) have not been diagnosed, suggests a large analysis of children and adolescents in Chicago conducted by investigators at DePaul and Northwestern universities.
The investigators screened 10,119 youth aged 5 to 17 from across 5,622 households in the Chicago metropolitan area. Families were first screened over the phone, and children with potential ME/CSF were brought to Lurie Children’s Hospital for in-person evaluations.
Of the initial 10,119 children, 298 were considered potentially positive for ME/CSF based on significant fatigue and a lack of other contributing medical conditions; 165 of these children were able to come in for an in-person clinical evaluation, of which 42 were given a positive diagnosis. Two of the 42 children had an existing ME/CSF diagnosis, which was confirmed.
Based on the samples, the researchers estimated a prevalence of pediatric ME/CFS at 0.75%, with higher rates among African American and Latin American children. “These findings point to the need for better ways to identify youth with this illness and to develop appropriate rehabilitation interventions for them,” the authors wrote in their study, which was published in Child & Youth Care Forum.
Jason LA, Katz BZ, Sunnquist M, et al. The Prevalence of Pediatric Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in a Community-Based Sample. Child Youth Care Forum. January 23, 2020 [Epub ahead of print]
Teen Use of Cannabis Associated With Depression, Suicide

Adolescents who use cannabis may be more likely to have depression and attempt suicide than adolescents who do not use cannabis, according to a report in Drug and Alcohol Dependence. Surprisingly, among cannabis users, those who used greater amounts of cannabis had lower rates of depression.
“While the present findings raise further questions about the relationship between severity of cannabis use and severity of depression among adolescents with cannabis use, clinicians should be aware that even remote cannabis use in an adolescent suggests a higher likelihood of depression,” wrote researchers from Johns Hopkins University and colleagues.
Their analysis of 2012-2017 National Survey on Drug Use and Health (NSDUH) datasets revealed that compared with adolescents who had never used cannabis, those with a history of use had higher odds of any lifetime depression, depression in the past year, or a suicide attempt in the past year. However, the relative odds of depression dropped as cannabis use rose.
Among teens with a history of use, those who had abstained from cannabis in the past year were 1.86 times more likely than never users to have had depression in the past year. This increased likelihood dropped to 1.66 times, 1.39 times, and 1.13 times among past year light users (1 day to 12 days), moderate users (13 days to 51 days), and heavy users (52+ days), respectively. Frequency of past year cannabis use did not affect the risk of past year suicide attempt.
“[O]ur findings could reflect heterogeneity in cannabis users, with some adolescents using for subjective relief of depression, and others using for social or other factors,” the authors wrote.
Gukasyan N, Strain EC. Relationship Between Cannabis Use Frequency and Major Depressive Disorder in Adolescents: Findings From the National Survey on Drug Use and Health 2012-2017. Drug Alcohol Depend. January 16, 2020. [Epub ahead of print]
Blue Light May Improve Sleep in Some TBI Patients

Sleep difficulties are a common symptom in people who have experienced a mild traumatic brain injury (mTBI). A study in Neurobiology of Disease reports that blue light therapy may help improve sleep and cognition in people recovering from mTBI.
Previous research has shown that exposure to blue light in the morning suppresses expression of the hormone melatonin, which speeds up the circadian clock and may promote earlier sleep the following evening.
Researchers at the University of Arizona conducted a seven-week clinical trial of 32 adults who had experienced mTBI within the past 18 months (but at least four weeks prior to their first assessment). After completing baseline neurocognitive assessments, each participant was randomly assigned to six weeks of blue light (active) or amber light (control) treatment each morning for 30 minutes.
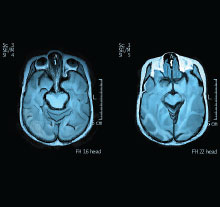
The participants also underwent MRI scans at the start and end of the study.
After six weeks, the participants who received blue light had reduced daytime sleepiness and improved performance on cognitive tests compared with those receiving amber light. The blue light participants also showed stronger structural and functional neural connectivity in brain regions connected to blue-light sensitive cells in the eye, suggesting the light was also accelerating neuron repair.
The study appeared in Neurobiology of Disease.
Killgore WDS, Vanuk JR, Shane BR, et al. A Randomized, Double-Blind, Placebo-Controlled Trial of Blue Wavelength Light Exposure on Sleep and Recovery of Brain Structure, Function, and Cognition Following Mild Traumatic Brain Injury. Neurobiol Dis. 2020; 134: 104679.
Social Deprivation During Infancy Has Enduring Effects on Brain
Severe social deprivation during infancy appears to have long-lasting effects on brain development, reports a study in PNAS.
While studies show early childhood deprivation is associated with higher rates of neurodevelopmental and mental disorders in adulthood, less is known of the impact of childhood deprivation on the adult brain.
Researchers at Kings College London and colleagues conducted MRI scans of 67 adults aged 23 to 28 who had been in Romanian orphanages during the Nicolae Ceaușescu regime (known for their significantly poor conditions) and subsequently adopted by families in the United Kingdom after the regime fell. Twenty-one U.K. adults who had been adopted but had no infant deprivation were also scanned as controls.
The Romanian adoptees had lower total brain volume on average than the controls, the authors reported. Among Romanians, larger reductions in brain volume correlated with more time spent at the orphanage; larger reductions in brain volume were also associated with lower IQ scores and more attention-deficit/hyperactivity disorder (ADHD) symptoms.
In contrast, the volume of the rear portion of their temporal lobe (a brain region involved in sensory inputs) was greater in deprived adoptees than those nondeprived, and these adults had fewer ADHD symptoms despite high reductions in total volume.
“The deprivation-related increase in right inferior temporal volume seemed to be compensatory, as it was associated with lower levels of attention deficit/hyperactivity disorder symptoms,” the authors wrote. ■
Mackes NK, Golm D, Sarkar S, et al. Early Childhood Deprivation Is Associated With Alterations in Adult Brain Structure Despite Subsequent Environmental Enrichment. Proc Natl Acad Sci U S A. 2020; 117(1): 641-649.



