APA Fall Conference to Focus on Determinants of Mental Health

On October 14 and 15, APA will host the successor to the Institute on Psychiatric Services: The Mental Health Services Conference (MHSC), to be held virtually. The conference theme is “Sociopolitical Determinants of Mental Health: Practice, Policy, and Implementation.” As a result of hard work and hours of study done by dedicated committees, the conference has been revamped to address evolving issues impacting patient care, deliver a more useful experience, and include more interaction between presenters and attendees. The reformatted conference will consist of plenary sessions, concurrent sessions, and deep-dive discussions.
Registration for the conference is now open at psychiatry.org/mhsc. The page is being updated with more details as we confirm the program sessions and speakers.
The MHSC Scientific Program Committee, chaired by Sarah Vinson M.D., includes Drs. Auralyd Padilla Candelario, Amy Cohen, Robert Cotes, Benjamin Druss, Jacqueline Feldman, Abhisek Chandan Khandai, and Sounmolu Shoyinka. As always, our lead administrative personnel—Leon Lewis, director of scientific programs, and his staff, Austin DeMarco, associate director; and Christopher Salazar, project manager—will provide their steadfast expertise for implementing the conference.
The topics on which the conference will focus include systemic trauma, structural racism, and health inequities. Additional topics will include integrated care in serious mental illness (SMI), the mental effects of climate change, mental illness and the criminal justice system, the special needs of indigenous and rural populations, and the impact of COVID-19.
Systemic trauma in communities will be the focus of several sessions. Trauma can consist of neighborhood violence, gun violence, mass shootings, police violence, and incarceration. These sessions will explore the policies that have been developed to address trauma as a social determinant of mental health, the level of success of those policies, and their practical application to improve resiliency within diverse populations.
Structural racism in the mental health care community will be another focus. In response to a reinvigorated national dialogue on structural racism, the American Association for Community Psychiatry has created a roadmap for community behavioral health providers that would (1) provide metrics specific to disparity and inequity issues in community behavioral health, (2) extend beyond cultural competency and linguistic appropriateness to incorporate structural inequity, and (3) promote a stepwise, concrete quality improvement process that can be adapted for self-directed use in community behavioral health settings. The Self-assessment for Modification of Anti-Racism Tool (SMART) will be introduced—this is a quality improvement tool that aims to facilitate organizational change in community behavioral health care.
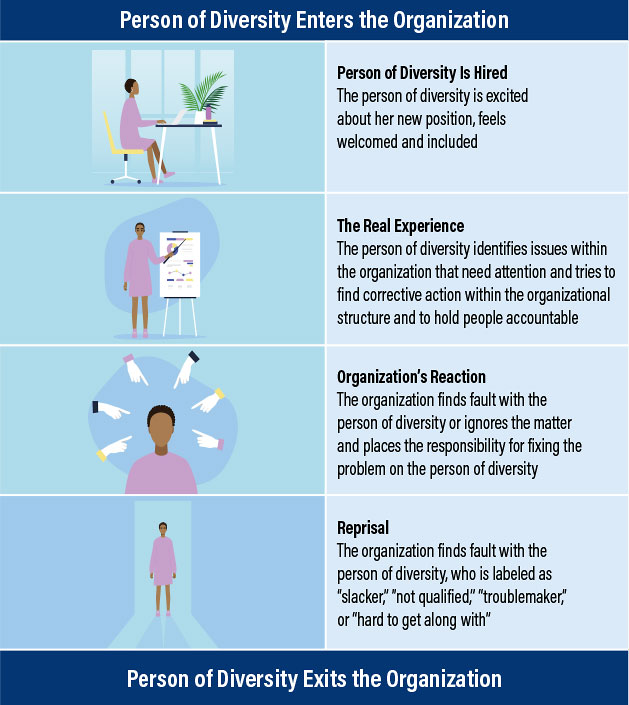
Discriminatory practices will be addressed in a session that examines disparities at several levels and their effects within APA, in hospital system training programs, and in the community (see infographic). Within APA, the voices of marginalized people need to be heard and recognized. Presenters will discuss the work that has been done so far, where we have fallen short, and where we need to go from here. In our hospital training programs, it is important to carefully evaluate and revise expectations and competencies for trainees to incorporate sociopolitical issues. Attention to these critical determinants of mental health early in training will help to improve the level of care that future clinicians can provide to the diverse patient populations under their care. Finally, in the community, we need to promote good behavioral health practice. We will introduce the key components of the SMART, describing our process in developing this organizational tool based on key inequity issues that are most relevant to community mental health practice. Lastly, we will use a case example to illustrate the process for using the SMART and describe future directions for piloting this framework.
Integrated care of those with SMI has an important role in reducing health disparities and achieving mental health equity for all patients. In integrated care practices, addressing the social determinants of mental health that impact our patients is critical to improving outcomes. With regard to social determinants related to race and ethnicity, peer supports and people with diverse backgrounds with lived experience with SMI have unique insights that we need to acknowledge and understand.
Climate change disproportionately impacts minority communities and is a driver of migration across the globe, undeniably a sociopolitical determinant. Addressing climate change and its impact on patients is an important aspect of ensuring quality patient care.
Criminal justice issues will be presented and will showcase how to work with police, patients, and detainees to avoid stigma, facilitate an optimal reentry into society, and prevent the injury or death of people with mental illness in crisis. Presenters will also explore the utilization of current systems and the systemic reforms that are needed to effectively treat patients within the criminal justice system.
Rural and indigenous populations are often overlooked and require unique and careful considerations to ensure quality care. Promoting mental health that emphasizes interdependence and holistic healing is critical for a culturally competent approach to caring for these populations.
COVID-19 has revealed a syndemic—biological and social interactions that increase a person’s susceptibility to harm or experience worse health outcomes. The September 2020 Lancet reported that infectious diseases such as COVID-19 were clustering within certain minoritized groups according to well-established patterns of inequality, especially in Black and Latinx communities. Presentations will discuss policy changes that should be considered to address and eliminate these kinds of systemic issues.
Lastly, I plan to initiate discussions at the MSHC about forming coalitions between different disciplines and from various sectors to work together to effectively advance patient care and address social determinants of mental health. Because of the intersectionality of social determinants of mental health, leaders in multiple disciplines engaged in frontline care, not just psychiatry, must work together more effectively than in the past.
I encourage you to register now for the MHSC for a stellar scientific, educational, clinical, research, and policy experience! ■
Learn more about the conference program and register here.



