A New Role for Interventional Psychiatrists: Ambassadors for Recovery
It is now April, and a year has passed since the first Interventional Psychiatry column appeared in Psychiatric News. When the column was first conceptualized, I thought that it would be a great venue to share information and the latest research findings on interventional treatments, highlight new and innovative treatments, and increase referrals to interventional psychiatry practices. Over the last year, however, I have begun to think that interventional treatments should be implemented because they are not only new and innovative, but also they lead to significant improvements in functioning and well-being. In other words, we should provide interventional treatments and refer to interventional treatments for superior patient outcomes, not just because the patient’s illness is not responding to conventional psychiatric treatments.
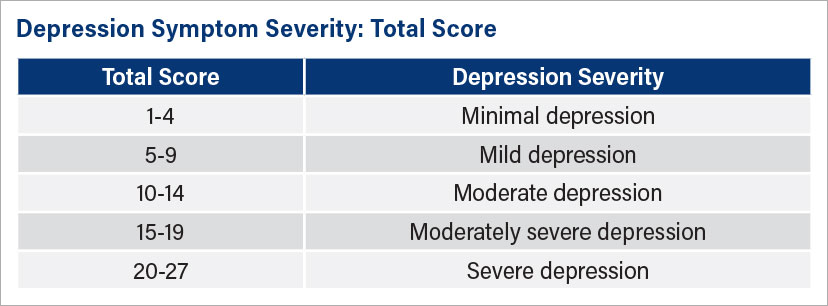
So how do we measure patient outcomes? Most interventional psychiatrists use a validated questionnaire to measure depressive symptoms (for example, the Montgomery-Åsberg Depression Rating Scale, Hamilton Rating Scale for Depression, and PHQ-9). When insurers first started covering transcranial magnetic stimulation (TMS), all required a baseline measure of depression with a validated questionnaire. Today most insurers require validated measures for monitoring symptoms while patients are receiving TMS, esketamine, and ECT. Although we like to complain about the insurance industry, I think the requirement to measure our outcomes has been a positive shift to improve quality overall and a big win for patients! Measures such as the PHQ-9 should be required to cover medication treatments and to monitor outcomes for all treatments including psychotherapy.
For patients with depressive symptoms, I use the PHQ-9. It is widely available; easy for patients to complete; in the public domain (“free”); and more importantly, used by many mental health and primary care clinicians. When I call a family practice physician or therapist and say, “Our patient had a PHQ-9 score of 25 at baseline, but after five treatments with esketamine, the patient’s PHQ-9 score dropped to 12,” the doctors get it! They understand the metrics because they have used the PHQ-9 with hundreds of patients.
When speaking with patients and families, I don’t speak in this manner, as it is meaningless from their perspective. Besides the total score, there are two other scores for items within the PHQ-9 that resonate with patients (see top box). Item 9 asks about dangerousness to self, self-harm, or suicide, and item 10 asks about the impact of the depressive symptoms on the patient’s functioning. For patients and their families, these two items might be more important than the total PHQ-9 depression score. Why would it matter if the depression score was 50% better, but there is still suicidal thinking (item 9) or significant impairment (item 10) at work?
Along with the total score and the individual elements that make up the questionnaire, I focus on items 9 and 10 and really try to understand the patient’s world of depression. Once I understand the patient’s world, I can most effectively assist the patient and choose the most appropriate interventional treatment. I can also paint a picture of recovery and appropriate expectations about what it is going to take to get there. Most of the time it is not just using an interventional treatment as monotherapy, but rather we integrate the interventional treatment with conventional medication management and psychotherapy.
Interventional psychiatrists are like psychiatrists who have subspecialized in other areas of psychiatry. We are ambassadors for patient recovery first! ■
Three Key Elements of PHQ-9 to Review With Patients
The Patient Health Questionnaire-9 can be used to understand how patients see their world. These are the major items to discuss with regard to depressive symptoms.
Item 9: Suicidality
Severity and frequency are rated numerically 0-3.
Item 10: Functional Impairment
Not difficult at all
Somewhat difficult
Very difficult
Extremely difficult
Depression Symptom Severity: Total Score
Communicating Depression Outcomes
In communicating with clinicians and with patients, I have several categorical outcomes that I try to highlight. The one that is meaningful and reachable for patients is recovery.
For Patients and Families
Clinical Improvement: 5-point reduction in PHQ-9 (depression severity) and improvement in Items 9 and 10.
“It looks like your depression is starting to improve. It looks like you are having reduced sadness and thoughts of self harm. You appear to be socializing more and having a better time with your family.”
Recovering: Total PHQ-9 score is 10, item 9 is 0, and item 10 is “not difficult at all.”
“It looks like you are recovering from depression and are having reduced sadness and no thoughts of self harm. It looks like you are socializing more and having a better time with your family. Although you are reporting some mild feelings of sadness, it appears to be less frequent and not impacting you at work or home or in your relationships.”
For Other Clinicians or Members of the Clinical Team
Response: 50% improvement in PHQ-9 score (depressive severity).
Remission: The almost total absence of any depressive symptom and no impairment in functioning. PHQ-9 <5.




