TMS Condensed! Rapid Acting With Improved Remission Rates With SAINT
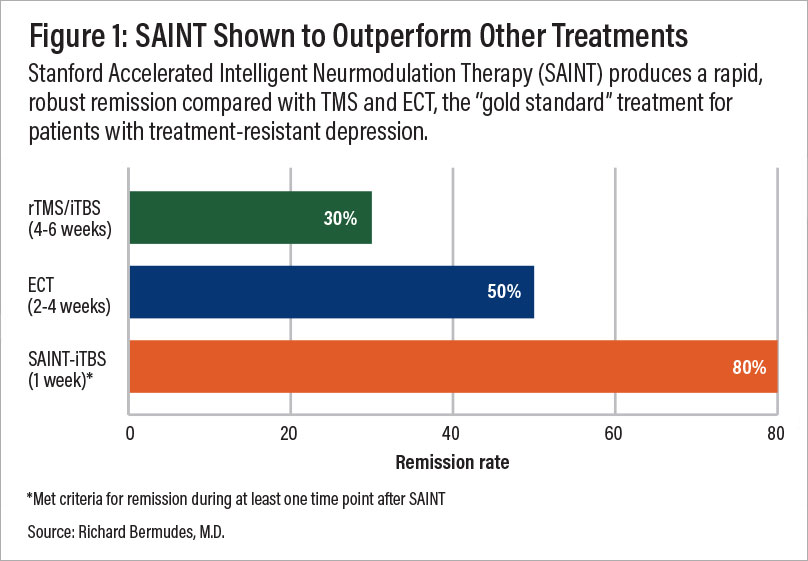
Thirty percent of patients with treatment-resistant depression (TRD) obtain remission with conventional repetitive transcranial magnetic stimulation (rTMS) or standard intermittent theta burst stimulation (iTBS) in four to six weeks. In a study posted in AJP in Advance on October 29, 2021, Eleanor J. Cole, Ph.D., and colleagues randomized 32 subjects with moderate to severe TRD to receive active or sham SAINT-iTBS for just a week of therapy.
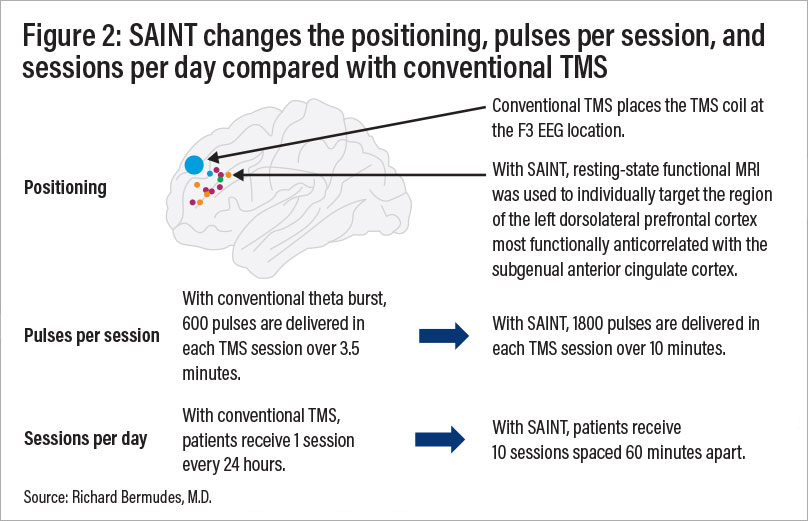
SAINT stands for Stanford Accelerated Intelligent Neurmodulation Therapy and is a new form of TMS that uses functional magnetic imaging (fMRI) to target the region of the dorsal lateral prefrontal cortex most functionally negatively correlated with the subgenual anterior cingulate cortex. With this new protocol, 10 sessions of active or sham SAINT-iTBS were delivered daily for a total of 18,000 pulses a day for five consecutive days. Each session lasted approximately 10 minutes; sessions were spaced 50 minutes apart so the average treatment day for each subject was just over 10 hours (see related article).
Overall, across the four-week follow-up, 12 participants, or 85.7%, in the active SAINT group met the criterion for response (a reduction ≥50% in MADRS score), and 11, or 78.6%, met the remission criterion (a MADRS score ≤10) in at least one of the five posttreatment assessments (see Figure 1). In the sham treatment group, four participants, or 26.7%, responded, and two, or 13.3%, remitted at some point during the four-week follow-up.
These results are impressive! Although a small study population, the safety profile is encouraging with no seizures, memory problems, or cognitive side effects. Headaches were more common in the active group, although most were relieved with nonprescription medications. Furthermore, the level of treatment resistance was moderate with most subjects failing five or more antidepressants or augmentation strategies previously, as well as two in the current episode.
So, is the future now? Perhaps, but several variables in the study were changed at once: (1) positioning, (2) number of pulses per session, and (3) number of sessions a day (see Figure 2). Thus, it is unclear which variable was the critical factor in the rapid and increased remission and response rates. It would be concerning if clinicians attempted to implement the protocol without the fMRI positioning, which is costly and not widely available. Furthermore, accelerated or high-dose TMS has not been shown to be superior to conventional TMS (C-TMS).
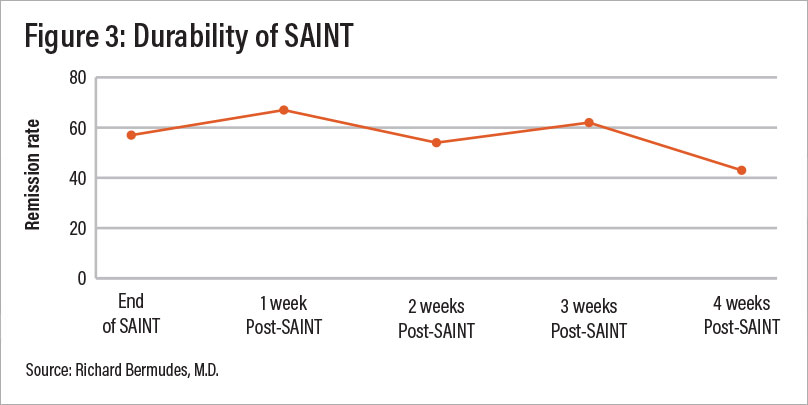
The durability of the response was monitored for one month after the last SAINT session (see Figure 3). During the study period, there was no other treatment offered, including C-TMS, pharmacotherapy, or psychotherapy. The durability of SAINT beyond a month and the best strategies to improve durability remain to be studied.
Patients and clinicians want rapid and durable remissions. This is a tall order for psychiatry. However, with this new form of TMS, we are a step closer. The FDA has granted SAINT breakthrough status, and the National Institutes of Health is funding a pivotal trial. The prospects of an 80% remission rate with a noninvasive brain stimulation treatment within five days is exciting news. One day SAINT might be used in inpatient settings to treat “depression brain emergencies.” ■
“Stanford Neuromodulation Therapy (SNT): A Double-Blind Randomized Controlled Trial” is posted here.




