Special Report: Youth With Eating Disorders—Time Is of the Essence in Achieving Remission
Abstract
Given that the symptoms of eating disorders may emerge over time and stay undetected even by loved ones and friends, early identification and treatment of children and adolescents are imperative.

Trivia time: imagine you are on a popular game show—you know, the one with the catchy theme song we can’t name due to copyright issues. The category “Psychiatric Disorders” comes up and you start to feel pretty confident you’ll get this one right. Suddenly, the clue is revealed: “This disorder has one of the highest mortality rates in all of psychiatry, with 12 times higher death rates in 15- to 24-year olds than any other cause.”
The theme show music starts as you rack your brain for the name of the disorder. The most deadly? By 12 times more? Your mind begins to race back through your coursework, trainings, clinical rotations, readings, and patient interactions, which leaves you with a number of potential answers. Perhaps major depressive disorder, or psychosis with command hallucinations, or substance use? Anything else? Aahh—time is running out. Quick, quick—what’s your final answer?
Did eating disorders come to mind? Because if they did, you would be correct (and hopefully win big in this fictional game show!). Eating disorders—in particular, anorexia nervosa—have one of the highest mortality rates of any psychiatric disorder, due in part to associated medical complications as well as an increased risk of suicide. Research suggests that 1 in 5 deaths from anorexia nervosa is the result of suicide. For children and adolescents, eating disorders are the third most common chronic health condition, behind only asthma and obesity in numbers. An estimated 1 in 30 people will develop an eating disorder at some point in life.
Eating Disorders Can Be Life Threatening Yet Underresearched
Eating disorders can severely impact just about every organ system in the body, including the cardiovascular system; cause diminished muscles, growth potential, and bone density; disrupt the endocrine and gastrointestinal systems; and can affect the brain. (Did you know the brain is the fattiest organ in the body?) While most of the medical complications of eating disorders resolve with improved nutrition and resolution of the eating disorder, not all damage is reversible, depending on the severity of symptoms and length of illness. Importantly, research suggests that after about three years of an eating disorder such as anorexia nervosa, for example, chances of full recovery diminish greatly. That’s three years from the onset of symptoms. Given that symptoms may emerge slowly over time and can stay undetected even by loved ones and friends, time is of the essence to identify and treat children and adolescents for eating disorders.
Despite these shocking statistics, eating disorder research has historically been significantly underfunded. For example, recent estimates of U.S. federal funding amounted to just $.73 per person impacted with an eating disorder, compared with almost $87 per person for schizophrenia and $59 per person for autism spectrum disorder. In Canada, estimates ranged from $0.11 to $0.61 per person impacted with an eating disorder, compared with nearly $47 for schizophrenia research and $54 for autism spectrum disorder. In addition, it can be challenging for patients and families to access expert medical and psychological care, which is often uniquely available in large, urban areas or in connection to academic medical centers. Access to telehealth options, videoconferencing platforms, and online treatments has helped alleviate this burden and broaden access to care, though finding qualified providers or programs with availability continues to be difficult. Obtaining training and certification in evidence-based treatment modalities also poses challenges for private practice or community-based providers who may not have convenient access to trainings and supervision needed to learn these treatments.
Our research team is currently exploring solutions to this hurdle by testing the effectiveness of online asynchronous clinical trainings in family-based treatment (FBT) for clinicians in private practice (NCT04428580; study still recruiting). Results of this implementation study as well as further work in this area will inform intervention training practices with the goal of improving access to expert, high-quality, and effective treatments for youth with eating disorders.
Fighting Myths and Misconceptions
Eating disorders represent a heterogenous category of diagnostic criteria, from restrictive undereating to disinhibited, overeating behaviors. And not all eating disorders are driven by concerns over shape and weight. In fact, avoidant restrictive food intake disorder (ARFID)—characterized by difficulty with maintaining adequate nutritional intake resulting in physical and psychosocial impairment—is not related to body image or weight concerns at all and can begin in much younger children. One shared trait that all eating disorders have in common? They are incredibly disruptive, distressing, and dangerous to the person suffering from one.
Although not every psychiatrist will be directly involved in providing eating disorder treatment, we all play an important role in recognizing the signs and symptoms of disordered eating while also disrupting myths about eating disorders that have become pervasive in today’s society. For example, it is not possible to look at someone and know the person has an eating disorder. A person’s outward physical appearance communicates little to no data about overall health. Moreover, eating disorders may impact anyone. Outdated myths that eating disorders affect only cis-gender, White, affluent females fuel harmful stereotypes and impede care for individuals who are suffering. Eating disorders are prevalent among gender-diverse youth and individuals who are from diverse racial and ethnic backgrounds. A 2011 study by Daniel Eisenberg, Ph.D., and colleagues in the Journal of American College Health found that 1 out of every 4 college students with an eating disorder identified as male. Another study by Michelle Goeree, Ph.D., and colleagues reported in a 2012 paper from the University of Zurich that female youth from low-income families were more than 150% more likely to have bulimia nervosa than female youth from high-income families.
Most important, eating disorders are not choices; they are not volitional. This is one of the biggest misconceptions about eating disorders. A teenager cannot simply wake up one morning and choose to have an eating disorder. Rather, there are strong biological and genetic influences that interact with individual differences, personality traits, neurobiological processes, and environmental contexts to result in an eating disorder. In our clinical care of adolescents with eating disorders, the number one question we get asked over and over is, “How did my child develop this? Where did it come from?”
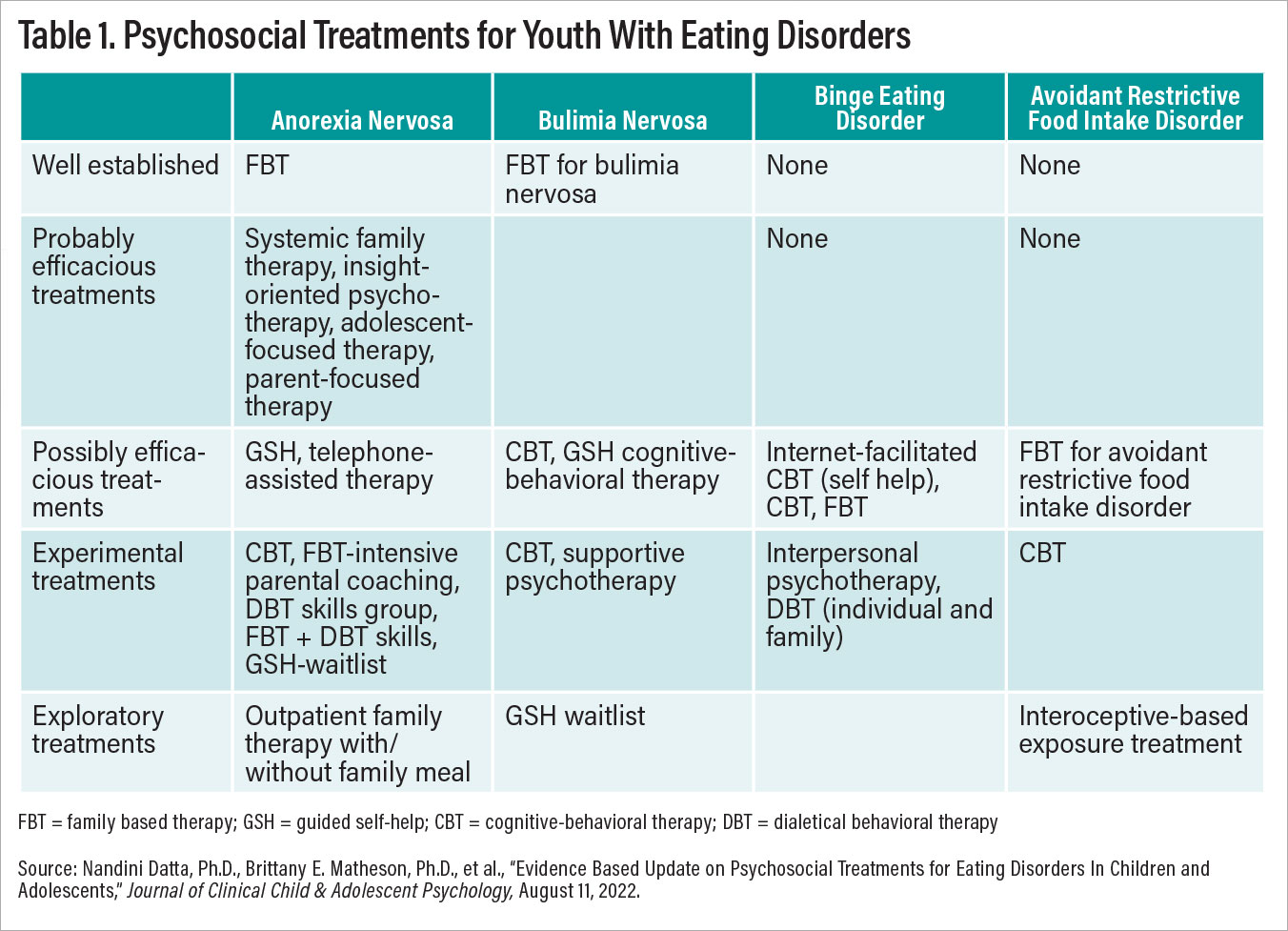
Table 1
The truth is that we don’t know. Research is underway to examine this very question, and perhaps one day, we’ll be able to posit a solution to this perplexing question. The good news is that we don’t need to know the “why” to treat patients with the disorder. And until we know more about the “why,” we encourage families to act quickly to help their young person overcome this terrible illness. Hemming and hawing over the “why” often delays families from focusing on the task at hand—and recovery from an eating disorder is a monumental task.
Sometimes we use the following analogy to help families better understand our “agnostic” stance. We might say, “Imagine you were just diagnosed with cancer. You are meeting with your oncologist and have just learned this devastating news. Would you ask your oncologist to hold off on talking about treatment options and therapeutic approaches until everyone figures out exactly how or why you got cancer?” Of course not. Instead, the conversation would immediately turn to treatment planning and next steps. An eating disorder diagnosis should be no different; the conversation must focus on how someone is going to start the recovery process. Although we may never truly understand the “why” for each individual patient, we do have effective treatment options for eating disorders in youth. And we need to get started right away.
Our team is composed of experts in the assessment and treatment of children and adolescents with eating disorders, and thus the information we present below is curated for this population. Importantly, there are key distinctions in the presentation and treatment options for youth compared with adults with eating disorders. For example, eating disorders in youth are more likely to be non-chronic and more responsive to intervention, and they rely heavily on family support in recovery efforts. We provide a brief overview of anorexia nervosa, bulimia nervosa, binge eating disorder, and avoidant restrictive food intake disorder with a tailored focus on the current evidence-based interventions as well as promising future research directions. These are also outlined for you in Table 1.
Anorexia Nervosa (AN)
Diagnostic criteria for AN includes restriction of energy intake driven by an intense fear of weight gain and shape/weight concerns. Individuals may be diagnosed with AN, restricting subtype (F50.01), or AN, binge-eating/purging subtype (F50.02). Common comorbidities include mood disorders, anxiety disorders, and obsessive-compulsive disorder. AN occurs across genders; socioeconomic statuses; and racial, ethnic, and cultural backgrounds, and it presents with the same preoccupations with weight, thinness, dieting, and overexercise that, if left untreated, results in significant medical consequences. Youth with AN require ongoing medical monitoring to ensure vital sign stability. With food restriction and malnutrition, all systems of the body are impacted, including the heart and brain. Common medical complications of AN include bradycardia—slowed heart rate, orthostatic changes in blood pressure from lying to standing, and electrolyte imbalances. At times, an inpatient hospitalization may be warranted for medical stabilization. AN has significant psychosocial implications for youth as well. Frequently, adolescents with AN withdraw from family and friends, becoming less social and engaged with their life outside of AN preoccupations.
Individuals who meet criteria for atypical AN report the same preoccupations with thinness, body image, and weight and engage in restriction, yet are not underweight by body mass index or growth chart standards. Not uncommonly, patients with atypical AN may also need to restore lost weight to promote vital sign stability and cognitive recovery from the eating disorder. The use of the word “atypical” is hotly debated and perhaps does not communicate the appropriate graveness and severity to families and clinicians.
For youth with AN, family-based treatment (FBT) is a well-established Level I treatment. It is the first-line treatment recommended by international guidelines and practice standards. In FBT, all family members who eat together in the home—parents/guardians, patient, siblings, even grandparents if applicable—attend hour-long outpatient treatment sessions with a certified therapist. FBT consists of three phases:
Phase 1, which consists of weekly sessions focused on parental involvement in renourishment, disrupting eating disorder behaviors, and establishing regular nonrestricting eating patterns.
Weight gain is often a target early in treatment, as research studies suggest that adolescents who gain 2.3 kg by session 4 of FBT have a 70% to 90% chance of achieving symptom remission by the end of treatment. Given that research trials of FBT typically achieve 40% to 50% remission rates, this marker of early response is critical for therapists, families, and patients to all work toward to promote improved outcomes.
Phase 2, which consists of biweekly sessions focused on transitioning independence with eating back to the adolescent while also working on social eating goals.
Phase 3, which consists of monthly sessions focused on an adolescent development task that the family has identified to work on together. The second session of FBT during this phase includes a family meal during which the family eats together with the therapist to learn new strategies to help the child overcome AN at mealtimes.
Adaptations and augmentations of FBT have been developed, including separate parent-only FBT and adding extra intensive parental coaching sessions for adolescents who do not respond to FBT within the first month of treatment. Based on clinical experience and supervision, virtual delivery of FBT looks quite similar to in-person treatment, though research studies have yet to directly compare outcomes across these two delivery formats. Guided self-help (GSH) adaptations for FBT are also in development, which, if found to be effective in adequately powered clinical trials, could significantly improve efficacy of treatment and reduce further barriers to accessing evidence-based care. Other evidence-based treatment modalities for AN are explored and briefly described in Table 1. More information about these treatment modalities can be found in our team’s evidence-based update for children and adolescents with eating disorders, published in the Journal of Clinical Child and Adolescent Psychology on August 11, 2022.
Bulimia Nervosa (BN)
The diagnostic criteria for BN include binge-eating episodes (loss of control eating plus consuming an objectively large amount of food within a discrete period of time) as well as use of compensatory behaviors at a frequency of approximately once a week for three months. Common comorbidities including mood disorders, obsessive-compulsive disorder, posttraumatic stress disorder, substance use disorders, and emotion regulation difficulties. Oftentimes, adolescents with BN report distress over their eating disorder symptoms and are typically more motivated to engage in care compared with adolescents with AN, given the egodystonic nature of BN.
FBT is a well-established outpatient treatment for adolescents with BN. Early response markers suggesting reduction in purging behaviors by session 2 and binge eating by session 4 may predict abstinence rates at the end of treatment. However, to date, there have been only four randomized clinical treatment trials for adolescent BN, with a total of 376 participants across the trials. As such, significantly more research is needed to replicate previous study outcomes as well as include a greater number of diverse individuals to improve generalizability.
Binge Eating Disorder (BED)
BED is the most commonly diagnosed eating disorder in adult populations, with a mean age of onset estimated to be about 23 years old. Individuals with BED report experiencing a sense of loss of control eating (LOC eating) while consuming an objectively large amount of food in a discrete period of time, often within two hours. Additionally, to meet diagnostic criteria, these eating episodes must be accompanied by marked distress and at least three of the following: eating rapidly; eating until uncomfortably full; eating when not feeling hungry; eating alone due to shame or embarrassment about how much one is consuming; and feeling disgusted with oneself, depressed, or guilty about the eating episode. Among children and adolescents, research has suggested that the experience of LOC eating correlates with anxiety, depression, marked distress, and poorer quality of life, independent of the amount of food consumed during these eating episodes. Prevalence estimates of LOC eating vary widely, from 8% to 30%, and may be greater among youth with obesity. LOC eating in childhood or adolescence may be a risk factor for the development of BED and/or BN.
To date, there are no Level I well-established treatments or Level II possibly efficacious treatments for binge eating in youth. Research studies have examined a range of treatment approaches within randomized clinical trials and small case series, including dialectical behavioral therapy, interpersonal psychotherapy, cognitive-behavioral therapy, and guided self-help cognitive-behavioral therapy. Evidence-based treatments for binge eating in adults may not directly translate to youth, given age and developmental differences as well as the child’s embedment within the family system. Thus, additional research into this area is needed.
Avoidant Restrictive Food Intake Disorder (ARFID)
A recently recognized eating disorder that was added to DSM in its fifth edition, ARFID is a selective eating disorder characterized by difficulties in maintaining adequate nutritional intake resulting in medical and/or psychosocial impairments. Individuals with ARFID do not express body image concerns despite engaging in restrictive eating behaviors, which uniquely separates this disorder from the others in the same category. Rather, eating behavior in ARFID is driven by three noninclusive subtypes: a lack of interest in eating/pervasively low appetite, sensory sensitivity (these kids know the difference between two seemingly identical boxes of Cheerios), and/or fear of aversive consequences such as vomiting or choking.
Individuals with lack of interest/low appetite presentation often present with longstanding histories of undereating and difficulties maintaining adequate intake, typically from very early on in life. It is not uncommon for youth with this presentation to forget to eat, be easily distracted by other activities, and report not feeling hungry. They may have difficulty receiving and interpreting internal hunger cues. Youth with the sensory sensitivity profile of ARFID report restrictive eating patterns based on sensory aspects of food and eating, which may include texture, temperature, smell, taste, color, or other aspects of appearance.
Children with ARFID may eat only a very narrow range of foods and often have strong preferences for specific brands or styles of food preparation. Varying from a preferred, known brand or preparation style may result in refusal to eat; for example, a child may eat chicken nuggets from McDonald’s without difficulty but will not eat chicken nuggets from other restaurants or those made at home. Children with this presentation may miss certain key nutritional elements due to their restrictive food range or may miss out on engaging in social events, such as birthday parties, traveling, sleepovers, family gatherings, or celebrations involving food.
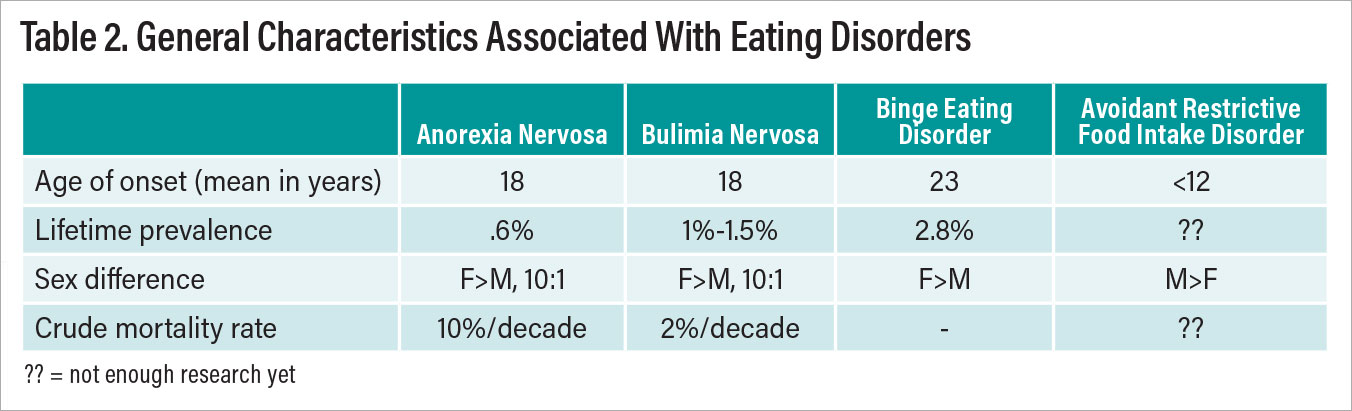
Table 2
For youth with fear of aversion consequences, their ARFID typically onsets after an event, such as choking on a hotdog, throwing up repeatedly due to food poisoning, or even experiencing pain while eating after orthodontic work. Children then become concerned about eating foods and may even go as far as to restrict all solid foods in an effort to avoid whatever unpleasant outcome they are afraid may happen after eating. This presentation often has a more rapid onset than the other subtypes and usually occurs later in childhood or early adolescence, though not always. Children with ARFID often don’t fall neatly into one of these categories, instead falling into two or even all three categories.
With any presentation of ARFID, families often feel significant pressure and stress regarding feeding their child. Parents can easily fall into the role of short-order cook. Also the adage “Your child will eat if hungry enough” simply does not hold true for many families’ experiences of a child with ARFID, particularly those within the low appetite subtype who will happily forgo eating. Parents report feeling frustrated, isolated, and guilty, fearful they have done something that caused their child’s eating difficulties. Parents may feel additional stress and worry if their child is not growing as expected or experiences medical complications stemming from their difficulties with eating, necessitating the consideration of enteral feeding. Although the recognition of ARFID as a psychological disorder is growing, it can still be missed or misdiagnosed by physicians who may assume it is a form of “picky eating” that the child will eventually outgrow without intervention.
Treatments for youth with ARFID are in development; the research is still in its infancy. To date, cognitive-behavioral therapy, FBT, and interoceptive-based exposure approaches have been explored in case series and small clinical trials. Our team is currently comparing FBT for ARFID with a psychoeducational and motivational treatment (PMT) in an adequately powered randomized clinical trial for children 6 to 12 years old (NCT04450771). This study is actively recruiting from a nationwide sample, with data collection underway; if you have patients interested in participating, please send an email to [email protected].
Key Takeaways and Next Steps
Eating disorders in children and adolescents represent a broad range of symptoms with various medical and psychological sequalae. It is important to act quickly and aggressively to treat these disorders before they become chronic or intractable. In youth particularly, eating disorders may threaten to disrupt windows for growth and opportunities for adolescent development and individuation. While many advances have been made in the past decade in treatment development and implementation, there is definite room for growth. There is an active effort to increase the diversity of youth in study samples to ensure cultural sensitivity and efficacy across diverse populations. We aspire to continue learning, developing, implementing, and disseminating treatment efforts to increase access to care and help treat youth with this dangerous category of illnesses. ■
References for Further Reading
Nandini Datta, Ph.D., Brittany E. Matheson, Ph.D., et al. Evidence Based Update on Psychosocial Treatments for Eating Disorders i3n Children and Adolescents. Journal of Clinical Child & Adolescent Psychology. August 11, 2022.
Daniel Eisenberg, Ph.D., et al. Eating Disorder Symptoms Among College Students: Prevalence, Persistence, Correlates, and Treatment-Seeking. Journal of American College Health. September 27, 2011.
Michelle Goeree, Ph.D., John Ham, Ph.D., Daniela Iorio, Ph.D. Race, Social Class, and Bulimia Nervosa. Working Paper, No. 86, University of Zurich, Department of Economics, Zurich, 2012.




