Journal Digest: Treatment-Emergent Mania, Fingerprint Scans, and More
Some Antidepressants May Increase Risk of Emergent Mania
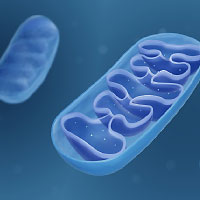
Some patients with bipolar disorder develop mania when taking antidepressants (known as treatment-emergent mania). A study in Molecular Psychiatry suggests that this risk may be higher when patients take antidepressants that increase activity in mitochondria—the metabolic engines of cells.
Researchers at the Mayo Clinic and colleagues looked at data from 692 patient records contained in the Mayo Clinic Bipolar Disorder Biobank, which collects longitudinal data on bipolar patients’ medication use and occurrence of depressive and manic episodes. The 692 individuals were selected because they were prescribed an antidepressant that has been shown in laboratory studies to increase mitochondrial activity (bupropion, nortriptyline, paroxetine, and venlafaxine) or decrease mitochondrial activity (amitriptyline and escitalopram).
The researchers found that treatment-emergent mania (defined as mania onset within 60 days of initiating an antidepressant or increasing an antidepressant dose) was almost twice as common in people taking a mitochondria-boosting antidepressant as those taking a mitochondria-decreasing one (24.7% versus 13.5%). After adjusting for differences in age, sex, and bipolar type (I or II) between the groups, the researchers found that mitochondria-boosting antidepressants were 2.2 times as likely to be associated with subsequent mania.
“[T]hese data suggest categorizing antidepressants based on mitochondrial energetics, and not solely on … conventional drug mechanism of action (SSRI, SNRI, TCA, MAOI), may be of value and warrant further consideration for future larger clinical and pharmacogenomic studies,” the researchers wrote.
Gardea-Resendez M, Coombes BJ, Veldic M, et al. Antidepressants That Increase Mitochondrial Energetics May Elevate Risk of Treatment-Emergent Mania. Mol Psychiatry. December 13, 2022. Online ahead of print.
EEG Data May Identify Patients at Risk of Delirium

A study in the Journal of the American Geriatrics Society reports that electroencephalography (EEG) scans obtained prior to a surgery may reveal which older adults are at greatest risk of delirium after surgery.
Researchers at the Hinda and Arthur Marcus Institute for Aging Research in Boston and colleagues collected EEG data from 20 older adults (average age 72 years) with no cognitive impairment about two months prior to an elective knee or hip surgery. The participants underwent a resting-state EEG scan followed by an EEG scan while the patient received brief transcranial magnetic stimulation (TMS) to assess the brain’s response to an environmental stressor.
Following surgery, three adults developed delirium (according to the confusion assessment method, or CAM criteria) during their hospital stay. All three of these adults had resting-state EEG readings well outside the range of the other 17 patients (two adults had much higher activity, while the third had much lower activity). All three adults also had elevated EEG activity following TMS, though only two of these patients had EEG activity outside of the range of non-delirium patients.
“Overall, our study suggests that noninvasive assessment of cerebral electrophysiology in patients scheduled for elective surgery is feasible, may reveal subclinical abnormalities in measures of cerebral connectivity and plasticity that indicate an elevated risk for post-operative delirium, and supports a theoretical framework of delirium as an interaction between endogenous cerebral vulnerabilities and environmental stressors,” the researchers wrote.
Ross JM, Santarnecchi E, Lian SJ, et al. Neurophysiologic Predictors of Individual Risk for Post-Operative Delirium After Elective Surgery. J Am Geriatr Soc. October 13, 2022. Online ahead of print.
Fingerprint Scans Offer Clues About Psychosis

Fingerprints may offer clues about people at risk of developing psychosis, a study in Schizophrenia Bulletin suggests.
Investigators at the FIDMAG Germanes Hospitalàries Research Foundation in Barcelona and colleagues recruited 612 adults aged 18 and older with a schizophrenia or schizoaffective disorder from 13 mental health hospitals across Spain, as well as 844 controls without either disorder. All participants were categorized as being of European-Caucasian ethnicity and had complete fingerprint scans done on both hands. The investigators then used machine learning algorithms to scan the prints for differences between the groups, both for individual fingers and multi-finger sets.
For individual fingerprints, analysis of the right thumb was most accurate at distinguishing a patient with schizophrenia from a control, with an accuracy of 68%; the right index finger had the lowest accuracy at 59%. Combined analysis of the left thumb, index, and middle fingers was 70% accurate at differentiating schizophrenia patients from controls.
“Although fitted models were based on data from patients with a well-established diagnosis, since fingerprints remain … stable after birth, our results imply that fingerprints may be applied as early predictors of psychosis,” the researchers wrote.
They continued, “[A] maximum accuracy of 70% does not provide enough precision for a faultless diagnosis, [but] fingerprint images may still be valuable, especially if they are combined with other sources of information that have already shown some predictive power in schizophrenia such as genetics and brain imaging data.”
Salvador R, García-León MÁ, Feria-Raposo I, et al. Fingerprints as Predictors of Schizophrenia: A Deep Learning Study. Schizophr Bull. November 29, 2022. Online ahead of print.
Buprenorphine Associated With More Favorable Neonatal Outcomes Than Methadone

Pregnant people with opioid use disorder who are treated with buprenorphine may experience a lower risk of neonatal complications (such as preterm birth) than those taking methadone, according to a study in the New England Journal of Medicine.
Researchers at Harvard Medical School and colleagues studied more than 2.5 million pregnancies recorded in a national Medicaid database between 2000 and 2018. This sample included 10,704 pregnant persons taking buprenorphine and 4,387 taking methadone during the first 19 weeks of pregnancy, as well as 11,272 taking buprenorphine and 5,056 taking methadone during the second half of pregnancy.
Compared with pregnant persons taking methadone early in pregnancy, those taking buprenorphine had a 42% reduced risk of a preterm birth, 28% reduced risk of an infant born a small birth size for gestational age, and 44% reduced risk of an infant born at low birth weight; these results were similar in persons exposed to buprenorphine or methadone during late pregnancy. Persons taking buprenorphine prior to the birth of the baby also had a 27% reduced risk of having an infant with neonatal abstinence syndrome compared to those taking methadone. There were no differences between the groups in the rate of maternal complications such as a caesarean section or delirium.
A follow-up analysis suggested that the differences in neonatal outcomes were not related to differences in the care that pregnant persons received when accessing buprenorphine versus methadone.
Though this study suggests that buprenorphine leads to more favorable pregnancy outcomes, “[a]ny opioid agonist therapy is recommended over untreated opioid use disorder during pregnancy, because untreated persons have greater incidence of adverse outcomes owing to withdrawal, return to opioid use, overdose, intravenous drug use, and inadequacy of prenatal care,” the authors concluded.
Suarez EA, Huybrechts KF, Straub L, et al. Buprenorphine Versus Methadone for Opioid Use Disorder in Pregnancy. N Engl J Med. 2022; 387(22): 2033-2044.
Psychosis in Depression Increases Suicide Risk

Individuals with psychotic depression are about twice as likely to die by suicide as individuals with severe nonpsychotic depression, according to a report in the Journal of Affective Disorders. The study also revealed that people with psychotic depression were more likely to die by violent means.
The researchers, from the University of Eastern Finland and colleagues, used Finnish health registers to identify all adults aged 18 to 59 years with a first diagnosis of severe depression with or without psychotic features between 2000 and 2018. Patient outcomes were then monitored for up to five years, death, or the end of the study in 2018.
The final sample included 85,989 individuals diagnosed with nonpsychotic depression and 17,331 individuals with psychotic depression. During the five-year follow-up, 2.6% of the individuals with psychotic depression died by suicide compared with 1.0% of those with nonpsychotic depression. After adjusting for different variables, the researchers calculated that people with psychotic depression had 2.19-fold increased risk of dying by suicide than people with nonpsychotic depression.
While the risk of suicide by any method increased among people with psychotic depression compared with nonpsychotic depression, the highest increased risk was observed for suicides of violent means. Compared with people with nonpsychotic depression, people with psychotic depression also had a slightly increased risk of accidental death from poisoning.
“Enhanced screening and monitoring for psychotic symptoms, such as paranoid ideas, delusions, and hallucinations is warranted for all patients with severe depression,” the researchers wrote. ■
Paljärvi T, Tiihonen J, Lähteenvuo M, et al. Psychotic Depression and Deaths Due to Suicide. J Affect Disord. 2023; 321: 28-32.



