Psychiatry Match Numbers Increase for 12th Consecutive Year
Abstract
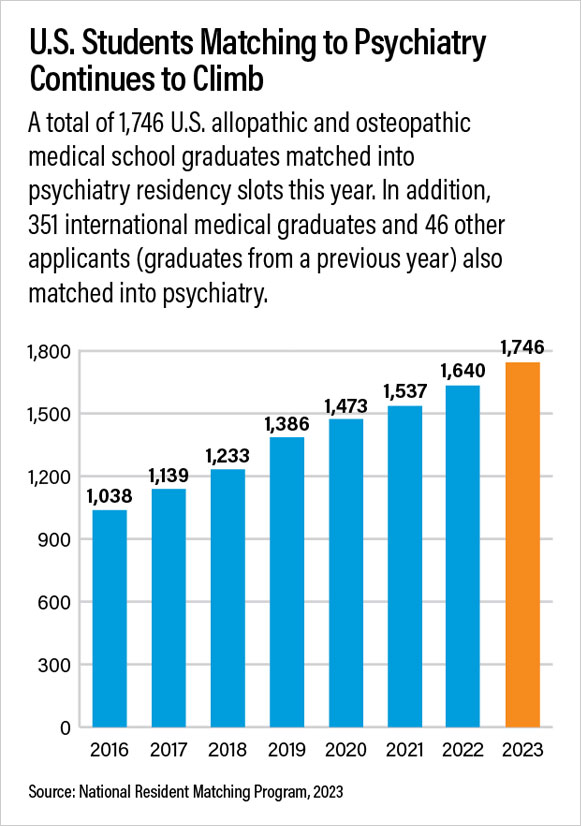
Psychiatry’s numbers have been increasing yearly since 2011. This year psychiatry was one of just 10 specialties with increases of more than 10% over the last five years.
A total of 1,746 U.S. medical school graduates—1,343 from allopathic schools and 403 from osteopathic schools—matched into psychiatry residency programs this year as part of the 2023 National Resident Matching Program (NRMP). It marks the 12th year in a row that psychiatry’s match numbers have increased.
Additionally, 351 U.S. and non-U.S. international medical graduates (IMGs) and 46 other applicants (allopathic and osteopathic graduates from a previous year) also matched into psychiatry, bringing the total to 2,143 medical school graduates. Just 21 psychiatry positions went unfilled.
The annual match, in which the program choices of graduating medical students are paired with those of residency programs seeking trainees, is typically watched as an indicator of workforce size and makeup of the various medical specialties for the coming years. Psychiatry’s numbers have been increasing yearly since 2011. This year psychiatry was one of just 10 specialties with increases of more than 10% over the last five years.
“There continues to be a sustained interest in psychiatric careers by both M.D. and D.O. medical graduates,” said Sidney Weissman, M.D., a former APA trustee and past president of the American Association of Directors of Psychiatric Residency Program Directors (AADPRT) who has been a longtime observer of workforce trends. “Their interest mirrors a heightened national focus on mental health and wellness. Since 2013 we have added over 130 new programs and 700 new positions in the match, and the number of U.S. senior medical students entering psychiatry has doubled. For the near term, these trends are likely to continue.”
Vishal Madaan, M.D., APA’s chief of education, said, “It is heartening to see such a successful match for psychiatry. I am delighted that our medical students continue to rise to the occasion and meet the challenge of growing mental health needs in our communities, especially in the post-pandemic world. Not only does psychiatry offer an opportunity for our medical students to answer the societal call and gain a better understanding of social determinants of mental health, but also it allows them to sustain a career that offers job security and quality of life.”
He pointed out, however, that the number of IMGs matching into psychiatry had declined from about 30% in 2013 to 16% in 2023, of whom just 6.9% are non-U.S. IMGs. “The number of IMG applications and matched positions, especially those for non-U.S. IMGs, continues to indicate a worrisome decline, creating potential workforce challenges for subspecialty recruitment and future public sector and rural psychiatry positions,” he said.
APA CEO and Medical Director Saul Levin, M.D., M.P.A., urged new residents to visit the APA webpage for resources for residents and medical students. “Mental health is now on the national agenda in a way it has never been before, and our profession is critical to meeting our country’s mental health crisis,” he said. “Psychiatry is an exciting field with an expanding array of effective treatments for mental illness. I welcome our new physicians in training and urge them to consider joining APA. Our trainees are our future.”
The NRMP is a private, nonprofit organization established in 1953 to oversee the match at the request of medical students to provide an orderly and fair mechanism for matching the preferences of applicants for U.S. residency positions with the preferences of residency program directors. The NRMP is sponsored by the American Board of Medical Specialties, the AMA, the Association of American Medical Colleges, the American Hospital Association, and the Council of Medical Specialty Societies. ■



