Xylazine Present in Increasing Number of Fentanyl Overdose Deaths, CDC Finds
Abstract
Xylazine was detected in more than 1 in 10 deaths involving illicitly manufactured fentanyl in June 2022.
Overdose deaths involving illicitly manufactured fentanyl where the veterinary tranquilizer xylazine (“tranq”) was also detected jumped 276% from January 2019 through June 2022, a study in Morbidity and Mortality Weekly Report has found. The results amount to a clarion call for rapid action on understanding the public health impact of xylazine and curtailing its further spread as an adulterant for other illicit substances.
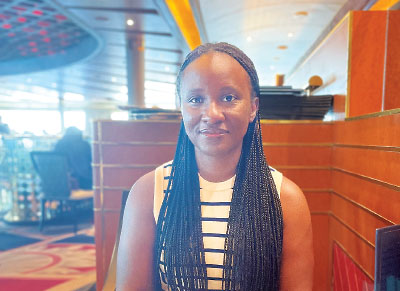
A lack of awareness about xylazine and its health risks makes it challenging to implement appropriate harm reduction measures, said Mbabazi Kariisa, Ph.D.
“Xylazine’s increasing presence in overdose deaths over time emphasizes the need for further investigation of its potency and effects on humans in order to clarify xylazine-related illness and overdose risks and inform prevention and response efforts,” lead author Mbabazi Kariisa, Ph.D., told Psychiatric News. She is a health scientist in the Division of Overdose Prevention at the Centers for Disease Control and Prevention’s (CDC’s) National Center for Injury Prevention and Control.
Kariisa and colleagues analyzed data from the CDC’s State Unintentional Drug Overdose Reporting System to compare monthly deaths involving illicitly manufactured fentanyl with and without xylazine as detected by postmortem toxicology testing. A drug was considered involved or co-involved if it was listed as a cause of death on the death certificate or medical examiner or coroner report.
“Postmortem toxicology testing results cannot determine which drugs were used simultaneously as separate products versus those that were mixed in one product and cannot determine timing of use. However, xylazine has a relatively short half-life of 25 to 30 minutes, which might indicate that if detected, it was part of the fatal drug use,” Kariisa explained. She added that determination of substance involvement may vary among individual medical examiners and coroners.
In 21 jurisdictions that included 20 states and the District of Columbia, the monthly proportion of deaths involving illicitly manufactured fentanyl with xylazine detected increased from 2.9% in January 2019 to 10.9% in June 2022. The number of deaths where xylazine was co-involved rose from 12 to 188 over the same period.
The researchers then expanded their analysis to include 32 jurisdictions spanning 31 states and the District of Columbia and narrowed the timeframe. They found that from January 2021 to June 2022, xylazine was detected in 9.0% of deaths involving illicitly manufactured fentanyl and co-involved in 6.9%. The highest percentages of deaths involving illicitly manufactured fentanyl with xylazine detected were in Maryland, Connecticut, and Pennsylvania, at 27.7%, 26.4%, and 23.3%, respectively. Compared with deaths without xylazine, a higher percentage of deaths with xylazine had evidence of injection drug use, 28.6% versus 19.5%.
Kariisa noted that toxicology testing for xylazine was not consistent across jurisdictions for the study period, which may have affected the study’s results.
“Detection of xylazine in overdose deaths is likely underestimated because some deaths where xylazine was actually present were likely classified as having no xylazine detected because it was not tested for,” Kariisa explained. “Because awareness of and testing for xylazine has increased in recent years, the scope of the increase might reflect increased testing as well as increased prevalence.”
Other Harmful Health Effects
Xylazine is legal only as a veterinary tranquilizer and is used mostly for sedating horses and animals in the Cervidae (deer) family. It has no approved use in humans.
“Limited studies suggest xylazine can cause central nervous system depression, respiratory depression, bradycardia, and hypotension in humans,” she said. “Additionally, chronic use of xylazine among some patients may be associated with other health effects, such as chronic skin ulcers or withdrawal symptoms.”

Although naloxone does not work on xylazine, it should always be given when an overdose is suspected, said APA President Petros Levounis, M.D., M.A.
Another challenge is that because xylazine is not an opioid, it will not respond to naloxone. However, naloxone should always be given when an overdose is suspected, including when xylazine may also be present, said APA President Petros Levounis, M.D., M.A.
“If patients tell you that they are using ‘tranq,’ think naloxone,” Levounis said. “It is much safer to assume that whatever they are using contains an opioid, likely fentanyl or one of the powerful fentanyl analogs.”
Tips for Reducing Health Risks
A lack of awareness about xylazine and its health risks makes it challenging to implement appropriate harm reduction measures, Kariisa said. She added that harm reduction tools such as xylazine and/or fentanyl test strips may not be accessible for all communities.
However, psychiatrists and other health professionals can work with patients directly to mitigate risk. To that end, Kariisa offered the following suggestions:
Talk to patients about the changing illegal drug supply, the risk of exposure to highly potent opioids like illicitly manufactured fentanyls mixed with xylazine, and the risk of overdose.
Counsel patients to call 911 should they witness a suspected overdose.
Advise patients that the effects of xylazine may continue after naloxone administration.
Provide active referral to treatment and care options and recovery support services, including wound care.
Implement post-overdose response protocols that incorporate links between public health, treatment professionals, community-based service organizations, and health care professionals. These protocols should promote overdose education, treatment, linkage to care, medications for opioid use disorder, and naloxone distribution.
The authors of this study did not report any outside funding. ■



