Ketamine Study Prioritizes Equitable Enrollment
Abstract
Researchers at Yale have secured $12.6 million for a study to compare the effectiveness of IV ketamine and esketamine for treatment-resistant depression. A priority of the study is to recruit patients from underrepresented groups to help ensure equitable access to these new treatments.
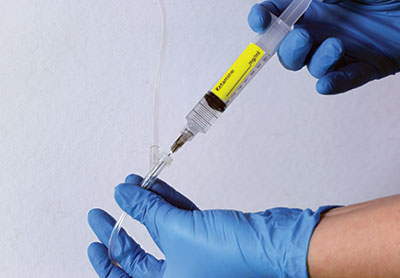
Though the number of for-profit ketamine clinics has surged over the past several years, the research behind ketamine’s efficacy and safety when delivered intravenously for psychiatric disorders is lacking. Yet with approval from the Food and Drug Administration (FDA), esketamine, delivered as a nasal spray (Spravato), boasts a voluminous body of data backing up its effectiveness for treatment-resistant depression (TRD).
“We have a unique case in which one version of this drug has an incredible amount of strong, well-controlled, rigorous data behind it, which is the case with intranasal esketamine. But clinically many sites are using the racemic version of ketamine intravenously, which does not carry FDA indication and for which we have much less high-quality data,” said Gerard Sanacora, M.D., Ph.D., the George D. and Esther S. Gross Professor of Psychiatry at Yale School of Medicine.
The similarity between IV ketamine (which contains both ketamine molecules, arketamine and esketamine) and the nasal spray Spravato (which contains only esketamine) and how effectively each could treat TRD has raised a lot of questions in the field of psychiatry, Sanacora explained. He and his colleague, Samuel Wilkinson, M.D., an associate professor of psychiatry at Yale School of Medicine, are aiming to answer some of those questions. They recently secured $12.6 million in funding from the Patient-Centers Outcomes Research Institute for a study in which they will compare the efficacy of IV ketamine and Spravato for patients with TRD.

Active community engagement is key for a new trial comparing IV ketamine and esketamine, said Lisa Harding, M.D. By engaging with communities through speaking at local events or working with community leaders, researchers can raise awareness and educate people about them, she said.
The trial’s primary outcome is the effectiveness of IV ketamine versus Spravato at four weeks, as measured by the 16-item Quick Inventory of Depressive Symptomology. Sanacora is hoping this head-to-head comparison will determine if the treatments are equivalent and if IV ketamine is noninferior to intranasal esketamine.
Sanacora and Wilkinson selected five sites (two academic sites and three community sites) from which 400 patients with TRD who are seeking treatment with either IV ketamine or Spravato will be recruited. The patients will be randomly assigned to receive one of the treatments and will report on their depression, anxiety, and satisfaction with treatment. An important aspect of the study, Sanacora explained, is the goal of recruiting a representative patient sample and ensuring patients from underrepresented backgrounds are included.
Including marginalized groups is crucial in all studies, said Lisa Harding, M.D., but especially in trials that test novel therapies. Harding is an assistant clinical professor of psychiatry at Yale School of Medicine. She also runs Depression MD, one of the three community sites participating in the study.
In an editorial published last year in The Journal of the American Academy of Psychiatry and the Law on regulating ketamine’s use in psychiatry, Harding noted that some prescribers may be less likely to recommend novel drug therapies to Black or Hispanic patients. To compound that problem, studies have shown that Black patients with depression are less likely to receive adequate treatment compared with White patients.
It is vital that Black individuals are included in clinical trials, but there is significant mistrust toward medicine within the Black community due to the history of medical experimentation, Harding said. “The question is, How can that mistrust be repaired?” she said. “Truly, the only way to gather data on how new treatments affect minorities is to include them in these trials. We—myself included as a Black woman—get caught in a Catch-22 because we were wronged by science and don’t trust it, but we also need science to ensure we aren’t left out of new treatment opportunities.”
The key to engaging patients from underrepresented groups is education and engagement, Harding said, particularly in this study. Patients with TRD have tried and failed on at least two antidepressants. They need education on why this clinical trial could be a good option for them and how IV ketamine and Spravato work. “Informed consent is incredibly important but often missing in everyday clinical practice,” she said. Educating primary care physicians is essential as well, she added, because patients are more likely to listen to someone with whom they already have a trusting relationship.
Sanacora and Wilkinson’s trial includes two clergy leaders from the African Methodist Episcopal (AME) Zion Church who are part of the Yale Cultural Ambassadors Program. Participants in the program help with trial recruitment, participate in community engagement activities, and help develop the protocols for trials, among other responsibilities.
TRD is a major problem throughout the world, Sanacora said, and there is a significant need for more treatments that will help these patients. “For many decades we really had only one class of antidepressants,” he said. “Now we’re at the point where we have different classes, and we have an opportunity to figure out if there are specific patients who are more likely to respond to one or another.”
Ensuring equitable access to these treatments is also paramount, he continued, and that means including historically underrepresented populations in trials. “If we’re not extremely cognizant and purposeful about how we develop these treatments, we could see disparities worsening,” he said. ■



