State Budget Woes Threaten Medical Care for the Poor
 Yet one more damaging result from the terrorist attacks of September 11 is surfacing in state governments throughout the country. The Kaiser Commission on Medicaid and the Uninsured reported that since those attacks, “the rate at which states’ fiscal conditions are deteriorating has accelerated, and many states have either made budget cuts or announced plans to do so.” Medicaid, the program on which the poor depend for their medical care, is a prime target for those cuts.
Yet one more damaging result from the terrorist attacks of September 11 is surfacing in state governments throughout the country. The Kaiser Commission on Medicaid and the Uninsured reported that since those attacks, “the rate at which states’ fiscal conditions are deteriorating has accelerated, and many states have either made budget cuts or announced plans to do so.” Medicaid, the program on which the poor depend for their medical care, is a prime target for those cuts.
The information, which appears in “Medicaid and State Budgets: an October 2001 Update,” is based on a telephone survey of 20 states conducted for the commission by the research firm Health Management Associates. An earlier study, “Medicaid Budgets Under Stress: Survey Findings for State Fiscal Years 2000, 2001, and 2002,” was being finalized when the attacks occurred. To provide the most recent information, the follow-up telephone survey included questions about budget changes since the attacks, possible reductions in Medicaid spending, and other actions to contain or reduce expenditures.
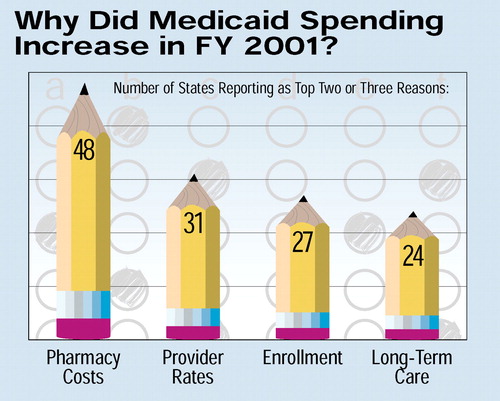
The impact of the attacks is exacerbating the problems of troubled economies in many states. In August more than half the states were either in recession or near recession, and Medicaid spending levels were already in jeopardy. The October update cites low growth projections for overall state budgets (2.4 percent), but “substantially higher projections for Medicaid [budget increases] (8.9 percent). . .putting renewed fiscal pressure on Medicaid.”
In fact, the survey found that in most of the 20 surveyed states, “Medicaid officials have been directed by the governor to prepare proposals to reduce the current year spending below the level authorized by the legislature.”
In Iowa, for example, a 4.3 percent across-the-board budget cut will reduce the state’s Department of Human Services budget, which includes Medicaid, by $38 million. Brian Cook, D.O., president of the Iowa Psychiatric Society, said, “The impact of the sagging economy is being felt in our ability to find placement options for patients on Medicaid and on the ability of patients to be certified as eligible for benefits. Reimbursement for psychiatrists is very low.”
In Georgia, proposals to cut Medicaid funds were due at the end of October for implementation by December. Officials reported, “We need to cut $88 million ($33 million in general funds) this year and $66 million in general funds next year.”
John J. Wernert, M.D., deputy representative of the Indiana Psychiatric Society, told Psychiatric News, “The Medicaid budget appears to be $200 million short. The governor’s solution has been to spread cuts throughout the Medicaid system, including payments to hospitals, nursing homes, and providers. We just learned that the state will end payment for housing in the community for Medicaid patients. Since state mental hospitals have been closed or downsized, many Medicaid patients will have no place to go but the streets.”
In Maryland, which was not included in the telephone survey, the mental health system was already “heading into a major crisis,” according to an article in the Washington Post. The article cites “soaring costs and chronic underfunding” as a source of a $150 million debt in Medicaid. The fallout already includes the bankruptcy of CPC Health Inc. and the closing of several clinics that serve Medicaid patients.
Current pressures for cost containment or reductions are heading for a collision with a more pervasive trend: the increased cost of prescription drugs. The Urban Institute estimates that Medicaid spending for outpatient prescribed drugs increased by an average of 18.1 percent per year from 1997 to 2000, compared with 7.7 percent for all Medicaid expenditures. The increase reflects both higher prices for drugs and an increase in the number of prescriptions used by beneficiaries.
Although data for those with disabilities (which include people with mental illness) are not separated from those for the elderly, those two groups account for a significant portion of the growth in prescription drugs and in Medicaid generally.
Medicaid is the largest source of public funds for mental health services. According to data from the federal Center for Mental Health Services (CMHS), as of 1997 the program was almost as important a source of funds for mental health and substance abuse treatment as was private insurance. Medicaid funds accounted for 20.3 percent of the total dollars spent on mental health and substance abuse, and private insurance accounted for 23.8 percent. The remainder came from other state and federal programs and out-of-pocket payments.
The impact of state budget cuts on the program is magnified because of federal funding formulas. According to the commission, on average for each $1 that states cut from their Medicaid budgets, the total amount of spending on the program drops by $2.33 because of the loss of federal Medicaid matching funds. And because the program is targeted to low-income people and those with disabilities, its importance increases when unemployment rises. Both the National Governors Association and the National Conference of State Legislatures have put forward proposals to increase federal spending on Medicaid during the current economic downturn.
Paul Appelbaum, M.D., APA’s president-elect, told Psychiatric News, “The prospect of substantial cuts in Medicaid budgets should be cause for great concern. Reimbursement levels will suffer, forcing more hospitals, clinics, and clinicians to avoid taking Medicaid patients. More states may be tempted to turn their Medicaid programs over to managed care companies, a trend that should be resisted since these entities often have shown themselves incapable of organizing reasonable systems of care.”
Nada Stotland, M.D., speaker of the APA Assembly, said in an interview with Psychiatric News, “It is heartbreaking to think that governments plan to balance budgets on the backs of those who are most poor and vulnerable. We want to reinvigorate APA’s commitment to those who have the most difficulty speaking for themselves.”
Assembly Recorder Prakash Desai, M.D., chairs an Assembly work group on public psychiatry that is charged with surveying states to identify existing standards for mental health services under Medicaid and with developing material such as an “issue kit” that can be used by psychiatric societies in states facing Medicaid cuts.
Reports from the Kaiser Commission on Medicaid and the Uninsured are posted on the Web site of the Kaiser Family Foundation at www.kff.org. ▪



