Govt. to Require Certification Of Opiate Addiction Programs
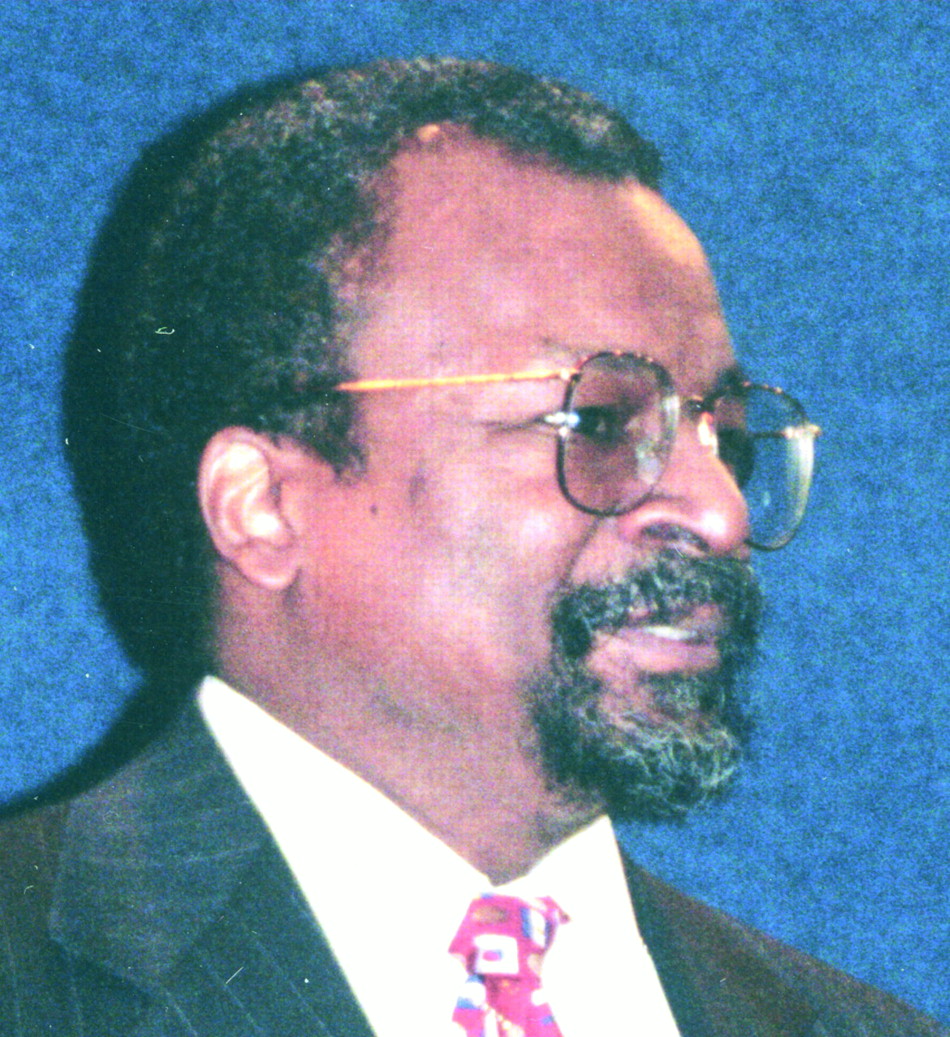
H. Westley Clark, M.D.: “The accreditation system will set a higher standard of care for those receiving methadone treatment.”
The new accreditation regulations will replace the nearly 30-year history of oversight of OTPs by the Food and Drug Administration with a streamlined system administered by CSAT.
Elements of the new accreditation regulations will be phased in over the next two years and will require any program that dispenses either methadone or levo-alpha-acetyl-Methadol (LAAM) to patients addicted to heroin or other opiates to obtain and maintain certification by one of several, but as yet unnamed, independent national accrediting bodies.
So far, two agencies are expected to be on that list, the Joint Commission for the Accreditation of Healthcare Organizations (JCAHO), which accredits hospitals and other acute-care facilities, and the Commission for the Accreditation of Rehabilitation Facilities (CARF). Both JCAHO and CARF participated in CSAT’s pilot study on accrediting OTPs. Other accrediting bodies may be added to the list, according to the regulations, which were published in the January 17 Federal Register.
The new accreditation regulations were to go into effect March 17, 2001, but are currently subject to President Bush’s hold order, pending the new administration’s review. CSAT Director
“The accreditation system,” Clark said, “will set a higher standard of care for those receiving methadone treatment. It should improve the quality of treatment programs overall by allowing for more clinical judgment in treatment, help to mainstream the medical treatment of opioid dependence, and continue a federal role, managed by CSAT.”
In anticipation of the new federal rule, CSAT developed new standards of care for OTPs. The standards mirror recommendations from the Institute of Medicine, the Congressional General Accounting Office, and the National Institutes of Health, which have sought to overhaul government control of methadone treatment for the last decade. Included in the standards, which emphasize improving the quality of care, are individualized treatment planning, increased limits for take-home quantities of medication, increased medical supervision, and required assessment of patient outcomes.
“Methadone has undergone more study than any other anti-addiction medication, with uniformly beneficial results,” said Acting SAMHSA Administrator
Suchinsky, who served as an advisor to CSAT during development of the new regulations, said that costs and documentation requirements are significant concerns of programs hoping to achieve accreditation. However, he said, “With CSAT’s technical assistance and hopes for funding assistance, they should not be insurmountable.”
The shift away from direct inspection of OTPs by the FDA to an accreditation approach managed by CSAT is expected to improve the quality of and access to narcotic addiction treatment programs. The new accreditation regulations only address methadone and LAAM dispensed through OTPs. Treatment options are expected to expand further under separate legislation that will allow office-based treatment by individual physicians using the partial opiate agonist buprenorphine (Psychiatric News, February 16).
According to Suchinsky, accreditation should allow for increased professional discretion and medical judgment in designing individualized treatment programs that are based solely on patient needs. For example, management of methadone or LAAM doses will be made on a case-by-case basis, as will determinations of the frequency and timing of therapy and counseling visits and options for whether and when a patient may attempt medically supervised withdrawal from medication.
Federal regulators also hope that the new standards will encourage state-of-the-art treatment services, with emphasis on outcome measures, especially those pertaining to reductions in crime and drug use, and engagement in productive employment. These changes are expected to enhance patients’ rights as well as outlining patients’ responsibilities.
“The new regulations,” commented
However, not everyone in the addiction treatment field is enamored of the new regulations. During the obligatory comment period prior to publication of the final rules, CSAT heard a significant amount of concern about details within the new accreditation process, including comments made during two public hearings on the issue last fall.
Critics of the plan expressed concern over the cost of obtaining accreditation, which the government estimated at $5,600 for the average OTP. Some testifying at the open hearings expressed concern that the costs would actually be much higher, considering that many of the nation’s 960 OTPs do not currently have the equipment or capacity to generate and maintain the appropriate records that would be required under the new system. Many testified that most of the existing programs are already cash strapped and would have a hard time coming up with the funds to initiate the accreditation process.
SAMHSA has pledged ongoing technical support for the programs and was looking for ways to help OTPs with the cost of the conversion to accreditation, whether it be through grants or direct offset funding for the accreditation fees.
Other concerns surrounded the failure of the new accreditation regulations to address the individual states’ regulatory authority over OTPs within their borders. Some who testified expressed fears that state regulations would supercede the new freedoms that are inherent in the accreditation system. CSAT officials noted, however, that the development of the new regulations was undertaken with the input of the state officials who oversee methadone clinics, downplaying any possibility of conflicting regulatory authority.
CSAT’s Clark told Psychiatric News: “We will work very closely with state regulators and individual programs throughout the country to make sure that each program has the support it needs to make this transition. Change is difficult, especially in the addiction field, and certainly within the regulatory environment. But what we are talking about here is a revolutionary improvement, centered on the needs of the patients.” ▪



