Psychiatric Care Threatened As States Seek Medicaid Cuts
The combination of rising health care costs and declining state tax revenues is straining an already overburdened Medicaid system.
And, next year, according to a survey of state Medicaid directors, the prospects for the program look even more bleak.
APA President Paul Appelbaum, M.D., told Psychiatric News, “Although Medicaid reimbursements are being cut and eligibility rules tightened, patients with psychiatric disorders will continue to need care. Many states employ the dishonest strategy of shifting the costs of that care to the psychiatrists and facilities that provide it. Coming on top of cuts in Medicare reimbursements and the ‘never pay retail prices’ approach of managed care, the new crisis in Medicaid threatens to destabilize the entire psychiatric care system.”
Chain Saw Needed?
Last month the Kaiser Commission on Medicaid and the Uninsured published “Medicaid Spending Growth: Results From a 2002 Survey.”
The document, which also includes interview results, contains these representative statements from Medicaid directors.
• “I don’t think there’s any light at the end of the tunnel yet. Our biggest problem is that a large part of the budget is funded by one-time funds.”
• “We won’t find needed savings on the margin. We’ll have to take a chain saw.”
• “The proposed cuts would be costly to the health care system in our state. When you look at the economic impact, it would be devastating.”
Forty-five states acted to contain costs in Fiscal 2002. At the time of the survey, additional cost-containing actions were planned in 41 states. According to the report, the “actual number will be greater. . .when mid-year actions are undertaken.”
Forty states plan a new control on prescription drugs in Fiscal 2003. Most frequently mentioned were greater discounts from pharmaceutical companies (26 states), more prescriptions under prior authorization (23 states), and implementation of preferred drug lists (22 states). Six states said they planned to limit the number of prescriptions a participant could fill each month.
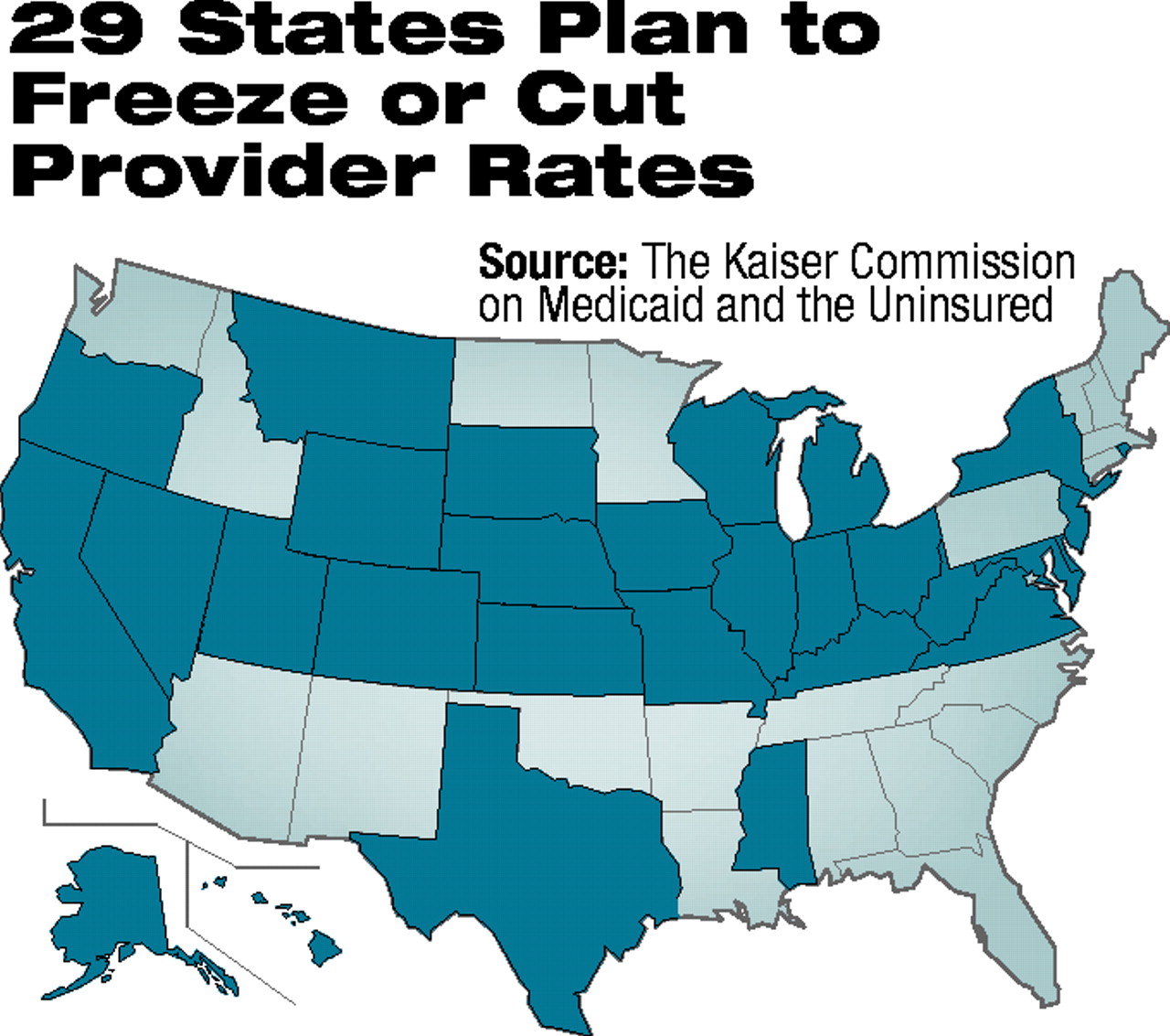
Twenty-nine states said that they plan to cut or freeze provider rates in 2003. Twenty states mentioned hospital rates, and 17 states mentioned physician rates. (States could mention more than one item.)
Funding Dilemmas
Exacerbating the problem of rising pharmaceutical costs, which affects both private and public health care, is Medicaid’s own Catch-22.
Medicaid rolls climb during troubled economic times. In fact, 39 states said that increased enrollment was one of the three greatest sources of Medicaid spending growth. Eighteen states cited increased enrollment as the most significant factor behind the state’s Medicaid spending increase.
Economic problems, however, also produce lower tax revenues and more competition for the use of those funds.
So, when the need for Medicaid programs and services goes up, usually the ability of states to pay for them goes down. And, since the flow of federal Medicaid funds requires some degree of matching with state dollars, each $1 cutback in state funds can trigger a loss of up to $2.33 in federal funds, at the highest match rate.
Altha Stewart, M.D., chair of APA’s Council on Social Issues and Public Psychiatry, told Psychiatric News, “Cuts in Medicaid budgets translate quickly into decreased access to quality care for the most vulnerable members of the population. Part of APA’s mission is to work to prevent that kind of harm to patients.”
Stewart thinks that it is important to establish coalitions with other advocacy groups at the state level and to find ways of educating members of state societies about successful advocacy with their state officials.
She said, “The level of support APA offers our district branches as they address the impact of declining public support for mental health will be extremely important. We need a public sector initiative that parallels the highly important work done in the private sector.”
On October 1 Sens. Max Baucus (D-Mont.) and Charles E. Grassley (R-Iowa) introduced legislation (S 3018) that would add $4 billion to the federal match for Medicaid, producing a 1.3 percent increase in payments to states over the next 12 months. It would also add $1 billion to Medicaid programs through block grants.
Jay Cutler, J.D., director of APA’s Division of Government Relations, told Psychiatric News, “This legislation is extremely high priority for APA in carrying out our advocacy mission for patients and the profession. We are extremely committed to ensuring there is no further destruction to a fraying safety net. We will find ways to help our DBs work together with all other patient advocacy organizations to address the critical importance of declining public support for psychiatric patients.”
“Medicaid Spending Growth: Results From a 2002 Survey” and related information are posted on the Web at www.kff.org/content/2002/4064/. ▪



