Models Point Way to Integrate Mental Health, Primary Care
David Pollack, M.D., and other Oregon state employees are using the state’s budget crisis to propel efforts to integrate mental health and primary care services.
Pollack, medical director of the Oregon Office of Mental Health and Addiction Services, told attendees at the annual meeting of the National Academy for State Health Policy in Portland that cutbacks in mental health coverage for people on the Oregon Health Plan (OHP) added urgency to the need for enhanced mental health services within primary care settings.
On March 1 the state cut outpatient mental health and substance abuse treatment benefits for 100,000 state residents who are eligible for the OHP but who do not meet criteria for mandatory Medicaid coverage.
He described the three models or approaches for integrating mental and primary health care, which the state is combining to produce a fourth model.
The Four Quadrant Model, which was developed by the National Council for Community Behavioral Healthcare, clarifies the roles and location of treatment, depending on the degree of severity of symptoms and of comorbidity.
Patients with low complexity and risk for both “physical” and mental health conditions, for example, are in quadrant one. They typically can receive mental health services in the primary care setting. In quadrant four are patients with high complexity for both “physical” and mental health conditions. They require the most specialized and comprehensive services.
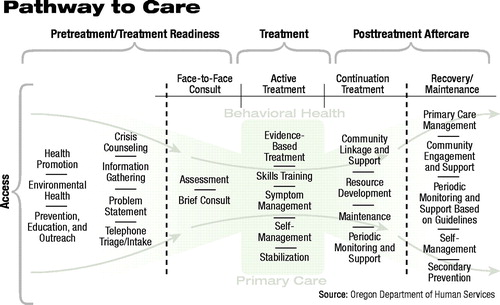 The Pathway to Care Model helps convey the range of treatment types and shows the similarities between the continuum of mental health and primary care services (see diagram).
The Pathway to Care Model helps convey the range of treatment types and shows the similarities between the continuum of mental health and primary care services (see diagram).
The model can be used to identify access, efficiency, and cost issues by highlighting gaps in the continuum. It calls attention to the importance of such activities as health promotion, crisis counseling, and community supports that are not always acknowledged in integration models.
The Chronic Care Model emphasizes the importance of an informed patient who knows about and can use strategies to manage his or her illness. Health care administrators organize resources to provide that support.
Care is delivered by a team of clinicians who work together to provide evidence-based treatment that includes an educational component for the patient and family members.
Successful implementation of any model or combination of models varies according to conditions at the local level, but it requires the completion of key tasks, said Pollack.
Administrators must complete an “environmental scan” to assess the pertinent resources and obstacles and gain “buy-ins” from administrative and clinical leaders whose support will be necessary.
They must make decisions about issues such as whether to contract for mental health services or employ mental health personnel directly.
Pollack told the group that both the federal government and foundations are promoting and funding activities that encourage integration of care.
He said, “The Health Disparities Collaboratives [HDC] project is one of the most exciting health care improvement programs going on anywhere.”
The HDC, which is funded by the Bureau of Primary Health Care at the Department of Health and Human Services, was developed to reduce disparities in health outcomes for poor, minority, and other underserved people by improving primary care practices.
It operates through community health centers to encourage collaboration on treatment for diabetes, asthma, cardiovascular disease, and depression and has developed training programs and other resources that are available at its Web site, www.healthdisparities.net.
The John D. and Catherine T. MacArthur Foundation is supporting the Initiative on Depression and Primary Care, with the aim of improving the quality of care for patients who have depression and are seen in primary care settings.
Information on the initiative is posted on the Web at www.macfound.org/research/hcd/mhp/depression_primary_care.htm. The Four Quadrant Model Background Paper is posted at www.nccbh.org. Information on the Chronic Care Model is posted at www.improvingchroniccare.org. The American Association of Community Psychiatrists’ position paper on mental health and primary care integration is posted at www.wpic.pitt.edu/aacp/finds/PCPMenu.html. ▪



