Candidate for Trustee-at-Large
About the Candidate
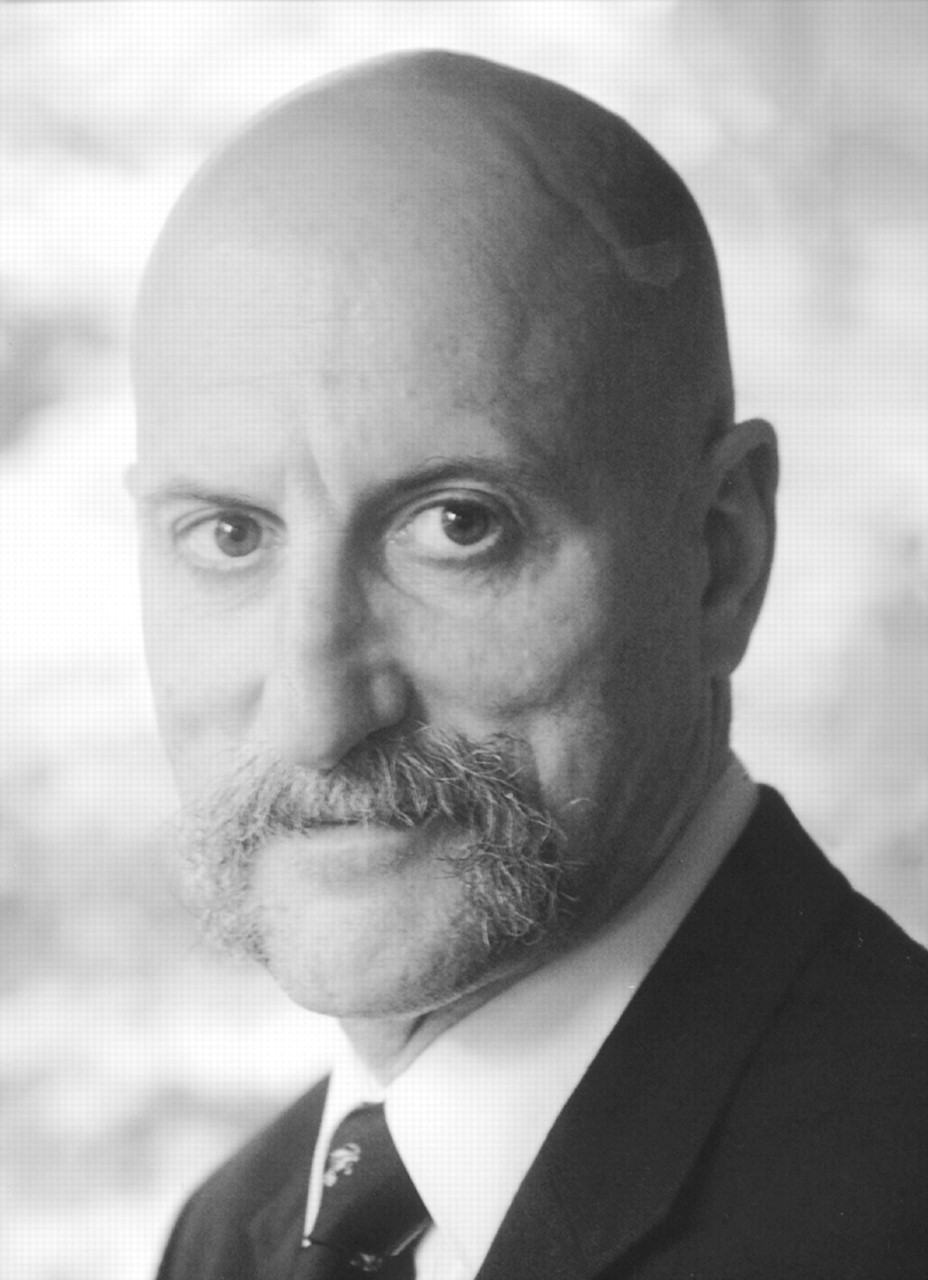
Distinguished Fellow (Member Since 1976)
| •. | Professor/Director of Public Psychiatry, University of Massachusetts, 1991- | ||||
| •. | APA Assembly: Area 1 Representative, 2002- ; Deputy Representative, 2001-02; Massachusetts Representative, 1993-2001 | ||||
| •. | Psychiatric Services: Editorial Board, 1992-2000; Column Editor, 1994- ; Book Review Editor, 1995- | ||||
| •. | Council on Global Psychiatry: Chair, 1999-2000; Vice Chair, 1997-98; Member, 1991-2002 | ||||
| •. | 2003 APA Van Ameringen Award for Psychosocial Rehabilitation | ||||
| •. | First Psychiatric Job: Recreational Aide, Gracie Square Hospital, 1968 | ||||
Candidates’ Views
Psychiatry in North America is in trouble:
| •. | The number of psychiatric beds is decreasing, while jail and prison beds are increasing at an annual rate of 3.5 percent | ||||
| •. | Medicare has announced a 4.2 percent decrease in M.D. reimbursement | ||||
| •. | Psychiatrists struggle under the burden of ill-defined terms that dictate clinical practice, such as “medical necessity” | ||||
| •. | “Consumers” are starving themselves to highlight their perception that psychiatry is based on faux science | ||||
| •. | Psychiatrists are undertrained and inadequately compensated for treating substance use disorders | ||||
| •. | Psychologists are in an absurd campaign to practice medicine; psychiatrists’ unreserved resistance is necessary, but costly | ||||
| •. | Parents are forced to relinquish custody of children to obtain necessary mental health services | ||||
| •. | There are 6,300 child/adolescent psychiatrists in the U.S. when more than 30,000 are needed; Canada has similar shortages | ||||
| •. | Despite clear need, there is general reluctance to pay for psychiatric care; rural areas suffer most in the U.S. and Canada | ||||
| •. | The right to consent to the release of personal health information is being circumscribed through HIPAA | ||||
| •. | Minority populations are underserved and ill served | ||||
| •. | In the past year, 29 states cut mental health funding; 35 states anticipate cuts in 2004 | ||||
| •. | The ranks of the uninsured increased by 2.4 million in 2002 | ||||
| •. | Private health insurance premiums increased 14 percent this year | ||||
| •. | Elderly individuals are pharmacologically tied up and physically tied down in nursing homes | ||||
| •. | The 1998-2002 sales of antidepressants increased 73 percent to more than $12 billion. Greater than 60 percent of all antidepressant prescriptions are written by primary care physicians | ||||
| •. | 75 percent of persons with serious mental illnesses report being discriminated against on the basis of their psychiatric disability | ||||
What I would try to help APA achieve:
Public Sector. APA should join the effort to actively work to end the IMD rule, the rule that prohibits Medicaid reimbursement for individuals in psychiatric hospitals.
Substance Use Disorders. APA should work toward an evidence-based explanation and the realignment of federal and state governments’ understandings of these disorders.
Youth. APA must work to increase the presence of child psychiatry in academia, stipends for child psychiatry residents, and reimbursement rates for collateral contacts.
Cultural Sensitivity. APA should focus part of its research agenda toward studies of differential treatment effects by race, gender, and ethnicity, and toward the consequences and remediation of mental health care disparities.
Health. APA, assisted by the AMA, must push to end discrimination against psychiatric patients in the delivery of all medical services.
Insurance. APA should be actively pursuing true parity by all insurers, including Medicaid and Medicare. Parity must include nondiscriminatory reimbursement for psychiatrists.
Advocacy. APA needs to vitalize the concept that until persons with mental illness are no longer seen as less worthy, equal opportunities and equal services will not be achieved.
Treatment. APA needs to refute the belief that psychotherapy and psychoanalysis provided by psychiatrists are anachronisms. APA’s research agenda must include studies of the cost-effectiveness of psychotherapy.
Research. APA must deliver its research findings to the public. Research findings should be informing all films and television productions.
You need to be part of the solution. It is time to get what our patients really need. Until we do that, we will never get what we really need: the opportunity to provide excellent treatment with reimbursement commensurate with our efforts. Our future and the future of our patients are one in the same.
Primary Loci of Work and Sources of Income
As professor and director of public sector psychiatry, I am full time at the University of Massachusetts Medical School, where I do administration, teaching, supervision, patient care, and research: 75% of income. On my own time I do state and agency consultation and other forensic work: 25% of income.



