No Short-Term Resolution in Sight For Malpractice Insurance Crisis
Protests by physicians in Pennsylvania, West Virginia, and elsewhere in the country over rising malpractice insurance fees appear to reflect a mounting crisis heralding a more vigorous call for tort reform.
And although psychiatrists do not appear to have been prominently involved in the most publicized protests—in which some physicians have threatened to stop work or cut back on services, and hospitals threatened to stop elective procedures and limit emergency room operations—experts in psychiatric liability say it is a crisis that affects doctors of all specialties.
“These protests reflect the tension among all physicians regarding malpractice,” said Alan Levenson, M.D. “Whatever their specialty and whatever their practice setting, physicians are feeling the impact of very significant changes in the medical malpractice world. Premiums are going up, carriers are pulling out of the market, and in many states they have stopped underwriting medical malpractice insurance. Other carriers are tightening up their requirements and restrictions relating to whom they provide coverage for.”
Levenson is president and chief executive officer of Psychiatrists Purchasing Group, which sponsors the APA-endorsed Psychiatrists’ Professional Liability Insurance Program (PLIP).
Approximately 7,000 members are covered under PLIP.
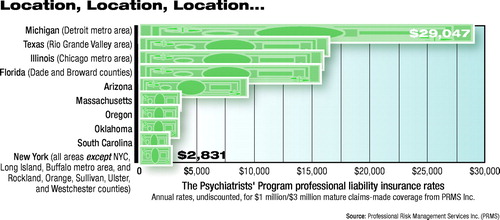 Levenson said premiums under the PLIP, after several years of stability, rose an average of 30 percent last year. He said the increase was related to market conditions affecting all of medical malpractice insurance. Rates vary markedly by geographic location (see graph). He added that for psychiatrists, the nature and setting of practice are critical. Those practicing in correctional facilities or community mental health centers—where the risk of malpractice is perceived as high—may be faced with especially steep increases in premiums, Levenson said.
Levenson said premiums under the PLIP, after several years of stability, rose an average of 30 percent last year. He said the increase was related to market conditions affecting all of medical malpractice insurance. Rates vary markedly by geographic location (see graph). He added that for psychiatrists, the nature and setting of practice are critical. Those practicing in correctional facilities or community mental health centers—where the risk of malpractice is perceived as high—may be faced with especially steep increases in premiums, Levenson said.
According to the American Medical Association, some specialties—including surgery and obstetrics-gynecology—are expected to experience increases of as much as 50 percent this year.
The crisis has also prompted a response from the White House. Speaking at the University of Scranton in Pennsylvania last month, President Bush lamented the litigiousness of American society and called for a $250,000 cap on noneconomic damages.
“Excessive jury awards will continue to drive up insurance costs, will put good doctors out of business or run them out of your community, and will hurt communities like Scranton,” Bush said. “And that’s why we need a cap on noneconomic damages, and that’s why we need a cap on punitive damages as well. . . .[I]t is the fear of unlimited noneconomic damages and punitive damages that cause docs and the insurance carriers to unnecessarily settle these cases. . . .In cases where more than one person is responsible for a patient’s injuries, we need to assign blame fairly. We need joint and several liability reform in our medical liability system.”
Million-Dollar Awards
Levenson and others say the steep increase in malpractice premiums across specialties appears to be related less to rising numbers of claims than to increasing costs for legal services and dramatic increases in jury awards—but also to complex factors related to the way the insurance industry does business.
The AMA cites research by Jury Verdict Research showing that in 1999 jury awards in claims cases jumped 7 percent in one year. In addition, it cost 30 percent more to settle a suit than it did just a year previously. About 45 percent of the 1998-99 jury awards were for $1 million or more, up from 39 percent during the preceding 12 months.
Martin Tracy, J.D., president and CEO of Professional Risk Management Services Inc., noted that while premiums are higher today than many physicians are used to, they are still lower in real dollars than they were 10 years ago.
Nonetheless, Tracy said that the crisis is real. During the late 1990s, when the economy was flush, insurance companies practiced “cash-flow underwriting”—using competitive pricing to attract enrollees, then using the premiums collected up front to invest in a bull market, he said.
“Today, diversified insurance companies can no longer anticipate double-digit investment income, so they are collecting more money up front,” he said.
He echoed Levenson in saying that the rising tide of malpractice premiums is lifting all boats. “I would not want to leave anyone with the impression that psychiatric malpractice exists in a special universe,” he said. “Most insurance companies that write malpractice don’t focus a lot on psychiatric malpractice as a separate entity, so when they raise rates, they raise them for all specialties.”
Levenson added that most major insurance carriers offer more than medical malpractice coverage, so they are affected by rising costs for other types of claims as well.
California Experience
Medical Insurance Exchange of California (MIEC) of Oakland, Calif., which insures approximately 1,000 psychiatrists, reports a 7 percent increase in premiums this year, due to many of the reasons cited by Levenson and Tracy. “Through the 1990s, premiums were stable or went down in California,” said MIEC Vice President Ron Neupauer. “But along with inflation we have seen an uptick in the number of large verdicts, while legal costs have also risen.”
MIEC is a physician-owned company that operates in five Western states.
Neupauer noted that physicians in California have benefited from the Medical Injury Compensation Reform Act (MICRA), passed in the wake of a malpractice crisis in that state in 1975. He says the law has “moderated the lottery system that occurs in other states in which a plaintiff can get a million-dollar award if [he or she has] a sympathetic jury.”
He explained that the law has four essential components: It caps noneconomic damages at $250,000, limits legal contingency fees along a sliding scales, allows offsets against a settlement if a plaintiff has other forms of recovery such as health insurance, and allows for future damages to be paid over time, instead of all at once.
Levenson and others say tort reform, such as California’s MICRA, is essential. “This is something APA and district branches need to be involved in,” he told Psychiatric News. “It is not only a national issue but a state one as well.”
In particular, Levenson said limits on noneconomic damages for pain and suffering were critical targets. Another area ripe for reform is that of “joint and several liability.” In a number of states, he said, a physician may be liable for a claim even though a hospital or other employer is also responsible. ▪



