Pendulum Swings Back To Specialty Training
Continuing a trend begun in the late 1990s, psychiatry registered another modest increase in the number of U.S. medical graduates entering psychiatry residency programs this year—one more sign, say workforce experts, that the “era of the generalist” is over.
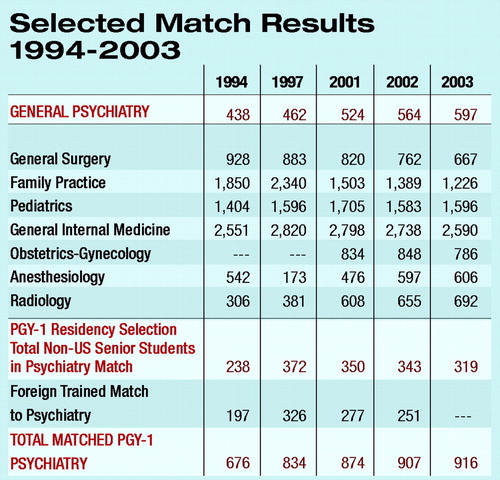 A total of 597 U.S. medical graduates filled psychiatry residency programs in this year’s “match,” conducted by the National Resident Matching Program (NRMP). That figure is up from the 564 U.S. graduates who matched into psychiatry last year, and the 524 students who chose psychiatry residency programs in 2001.
A total of 597 U.S. medical graduates filled psychiatry residency programs in this year’s “match,” conducted by the National Resident Matching Program (NRMP). That figure is up from the 564 U.S. graduates who matched into psychiatry last year, and the 524 students who chose psychiatry residency programs in 2001.
Conducted annually, the NRMP is the system that matches the program preferences of applicants with the preferences of residency programs that offer available training positions at U.S. teaching hospitals.
APA leaders familiar with psychiatric workforce issues welcomed this year’s numbers, saying they demonstrate the attractiveness of the profession to America’s future physicians. And they say it demonstrates the waning of the “generalist initiative” that began in the early 1990s, when primary care gatekeepers were seen as essential in a future dominated by managed care.
“It’s very good news,” said Frederick Sierles, M.D., past chair of the psychiatry workforce coalition—a group including representatives from APA, the American Association of Directors of Psychiatric Residency Training, and other organizations. “This is essentially the fifth consecutive year there has been a distinct increase in the number of U.S. seniors going into psychiatry. In part it has to do with the decline in medical student selection of primary care specialties, particularly family medicine.”
According to the NRMP, family practice experienced the sixth straight annual decline in the number of U.S. graduates choosing family medicine residencies. From a high of 2,348 U.S. graduates entering those residencies in 1997, the number fell this year to 1,226. The number of U.S. graduates entering internal medicine also declined again, from 2,738 in 2002 to 2,590 this year.
Meanwhile, psychiatry and other specialties—including some, like anesthesiology and diagnostic radiology, that were considered all but moribund a decade ago—continued to garner increasing numbers of U.S. graduates.
But Sierles believes the modest but steady increase in students choosing psychiatry also reflects the growing attractiveness of a profession that combines a relatively good salary with an expanding research and clinical knowledge base and the opportunity to spend time with patients.
“It has to do with the attractiveness and desirability of psychiatry itself, apart from the waning of the generalist initiative,” he said. “Psychiatrists are able to spend more time with patients than any other specialists. Jobs are relatively more available, and the field is developing.”
Sierles is a professor of psychiatry at Finch University of Health Sciences/Chicago Medical School.
Sydney Weissman, M.D., director of residency training in the department of psychiatry at Northwestern University School of Medicine in Chicago, agreed that psychiatry is reaping the rewards of a decline in interest in primary care.
“The generalist movement is history,” he said. “Primary care has not caught on in the United States. Psychiatry has recovered to levels it had in the early 1990s, while we have seen family practice numbers collapse.”
But Weissman said psychiatry will continue to face challenges in the future, stemming from rising health care costs and the shrinking health care dollar. “In light of changes in health care delivery and reimbursement, I do not see the likelihood of major increases in recruitment into psychiatry in coming years,” he said.
He said that the very nature and identity of psychiatry in the future remains a question that will influence student choices: Will psychiatrists be doing psychotherapy? Or will they principally be psychopharmacologists?
Weissman said the number of U.S. students entering special double- and triple-board programs in psychiatry continues to be insignificant. “Looking inside psychiatry’s recruitment of U.S. medical graduates, we continue to see limited interest in internal medicine-psychiatry programs and family medicine-psychiatry programs,” he said. “The psychiatry triple board survives but with limited interest. In 2003 no U.S. graduates matched into psychiatry-neurology programs. Students would appear to see both specialties as quite different, even though they both deal with the brain function.”
Despite a shortage of child psychiatrists, no students matched into combined general psychiatry and child programs while in medical school, according to NRMP statistics.
“If combined programs are going to be useful in enhancing recruitment into child psychiatry, much more work will need to be done,” Weissman said.
As in past years, the great majority of psychiatry residency slots not filled by U.S. medical graduates will be filled by international medical graduates.
A total of 319 students who did not graduate this past year from U.S. medical schools matched into psychiatry this year, according to the NRMP. In addition to non-U.S. citizen graduates of foreign medical schools, that figure also represents Americans who trained overseas, Canadians, osteopaths, former U.S. graduates who took time off between graduation and entering the match, and students in a handful of other categories. At press time, the NRMP did not have a breakout for each category, but in the past the overall figure has largely comprised international medical graduates who were not U.S. citizens.
A total of 986 psychiatry positions were offered through the match this year, with 916 (comprising the 597 U.S. graduates and 319 students who did not graduate this past year from U.S. medical schools) positions filled, according to the NRMP. ▪



