Medicaid Embraces Managed Care As Private Insurers Turn Away
The use of managed care strategies and techniques in Medicaid programs is accelerating, although the trend in the private sector is heading in the opposite direction.
In “Medicaid Managed Care: The Last Bastion of the HMO?,” Debra A. Draper, Robert E. Hurley, and Ashley C. Short reported growth in absolute numbers of Medicaid beneficiaries and in the percentage of beneficiaries receiving services through managed care companies.
Between 1990 and 2002, the Medicaid population expanded by nearly 60 percent to more than 40 million beneficiaries.
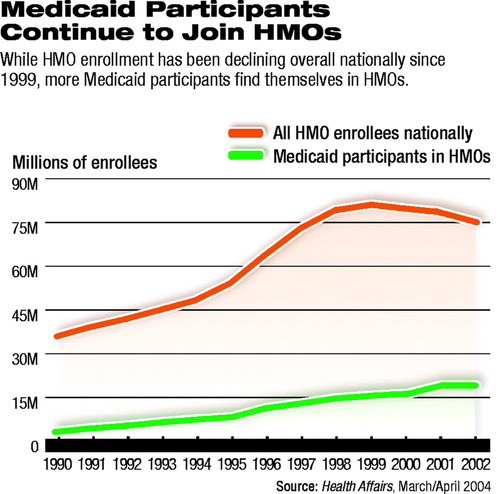 Twenty-three million of the 2002 beneficiaries were enrolled in managed care plans, a 10-fold increase in the number since 1990 (see chart).
Twenty-three million of the 2002 beneficiaries were enrolled in managed care plans, a 10-fold increase in the number since 1990 (see chart).
The study appears in the March/April Health Affairs.
Using qualitative data from the Community Tracking Study (CTS), a study conducted by the Center for Studying Health System Change, the authors also identified emerging trends in states’ administration of Medicaid benefits.
The CTS, which is funded by the Robert Wood Johnson Foundation, is based on interviews with key informants about health care in 12 metropolitan areas every two years. The authors used information from the most recent round of site visits, conducted between September 2002 and May 2003, as well as from the three previous rounds.
Conventional insurance companies, such as Aetna and Blue Cross of California, are exiting the Medicaid market. Their places are being taken by health plans that focus primarily on Medicaid and are often operated by health care providers, such as hospitals.
According to the authors, these plans “rely extensively on the traditional tools of managed care, such as primary care gatekeeping, prior authorization, and concurrent review, [an approach that] differs greatly from the commercial HMO sector, where there has been extensive movement away from restrictive product designs in recent years.”
Plan administrators depend on these restrictive tools because federal law prohibits Medicaid programs from using some cost-saving strategies that can be used by the private insurance market.
Copayments must be kept low in Medicaid, for example. The benefit package cannot be diminished below what is stipulated by federal legislation.
The shift to Medicaid-focused plans raises policy implications for states, the authors noted.
Administrators of plans that have exited the Medicaid market cited concerns about payment rates that do not reflect rising costs and about “inadequately funded program requirements.”
Those concerns suggest that states might have difficulty maintaining participation by the plans that are newcomers to the Medicaid market.
APA past president Paul Appelbaum, M.D., commented to Psychiatric News that because of the differences between Medicaid and the private insurance market, low-income and disabled groups are “disproportionately subject” to cost-containment strategies that wealthier populations have resisted successfully, despite the fact that Medicaid beneficiaries are more likely to have chronic disorders.
He noted that Medicaid is inadequately funded and added, “The externalized costs are born by the patients themselves and by the providers that are reimbursed at a rate that sometimes is below the cost of delivering care.”
It is unclear whether Medicaid beneficiaries have been hurt yet because of the use of “restrictive tools” by the Medicaid-focused plans and by the exit of conventional insurance companies from the market.
Selby Jacobs, M.D., predicted that for mental health clinicians and patients, “aggressive utilization management will pose a challenge.” He also noted that the narrow choices offered to patients by these plans could become a problem.
Jacobs chairs APA’s Committee on Public Funding for Psychiatric Services.
Appelbaum suggested that increased managed care in Medicaid likely will promote “more carved-out mental health care, with all the problems that brings—fragmentation of care, disincentivization for primary care providers to address mental health issues, and further diversion of financial resources to profit-making entities.”
“Medicaid Managed Care: The Last Bastion of the HMO?” is posted online at http://content.healthaffairs.org/cgi/content/full/23/2/155. ▪
Health Affairs 2004 23 155



