When Elderly Are Depressed, Family Faces Care Burden
Elderly people with depression require a significant and costly amount of regular care and assistance provided by family members.
The additional hours of “informal care” attributable to depressive symptoms—over and above the amount of informal care typically provided for elderly people—represents a significant time commitment for family members and societal economic cost, according to the May American Journal of Psychiatry.
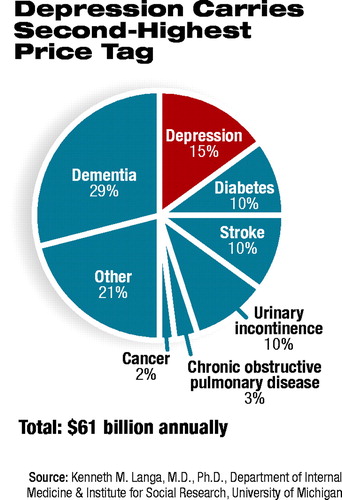
Study author Kenneth M. Langa, M.D., Ph.D., told Psychiatric News that based on similar studies of other conditions in the elderly (including cancer, diabetes, urinary incontinence, among others), depression ranked second only to dementia in the amount of additional care required by family and other informal caregivers.
“Most psychiatrists have a sense that depressed people will need to depend on the people around them,” he said. “What is significant is that this is the first study that quantifies the amount of care associated with depression in older people.”
Langa is an assistant professor of medicine at the University of Michigan School of Medicine.
He said that while the amount of time spent on a per-person basis (approximately three extra hours a week) may not seem significant, the prevalence of depression in the elderly makes the cumulative amount of required informal caregiving enormous at a national level. Caregiving associated with depressive symptoms in elderly Americans represented a yearly cost of about $9 billion, according to the study.
Elderly women were more likely than elderly men to report depressive symptoms. Seventy-three percent of women, compared with 23 percent of men, reported four to eight depressive symptoms in a week. Sixtyfive percent of women, compared with 35 percent of men, reported one to three depressive symptoms in a week.
In a previous study by Langa and colleagues, women with functional limitations received significantly fewer hours of informal care than men with similar levels of impairment The study, “Gender Disparities in the Receipt of Home Care for Elderly People With Disability in the United States,” appeared in the December 20, 2000, Journal of the American Medical Association.
“It is important for psychiatrists and other clinicians to know that older women who live alone may be at heightened risk for depression, yet may receive significantly less care than men,” he said. “They are much more likely to be living alone, and even when they are married, they receive about half as much help as their spouse.”
Langa said the study has important implications for policymakers. Though informal care can be considered “off the books” of public and private insurance ledgers, it nevertheless represents a significant hidden cost to society.
“The costs of depression are not confined to the direct costs of treating the condition or of suicide,” he said. “There is a significant cost that spreads out to the family. That's important to consider in policy debates.”
In the study, data from the 1993 “Asset and Health Dynamics Among the Oldest Old Study,” a nationally representative survey of people age 70 years or older, were used to determine weekly hours and cost of informal caregiving for 6,649 respondents. Forty-four percent of the respondents reported one to three depressive symptoms, and 18 percent reported four to eight depressive symptoms.
Adjusting for sociodemographics, caregiver network, and coexisting chronic health conditions, people with no depressive symptoms received an average of 2.9 hours a week of informal care, compared with 4.3 hours a week for those with one to three symptoms, and 6.0 hours a week for those with four to eight symptoms.
Costs of informal care were estimated by using a range of costs associated with buying home health care for their depression and other chronic conditions. The annual cost nationally of $9 billion for informal care for depression compares with $6 billion each for stroke, urinary tract infection, and diabetes. For dementia, costs of informal care are $18 billion, according to Langa.
“Clearly, the brain is important,” he said. “Dementia, depression, and stroke are the most costly in terms of informal care.”
Langa said the specific pathways by which depression leads to increased requirements for informal caregiving are deserving of further study.
“The most likely hypothesis is the anhedonia associated with depression,” he said. “People with depression are not really interested in things and have trouble getting up. Family members are required to get the depressed individual up and going.
“There is also the issue of the interaction with other chronic conditions. Someone with severe diabetes who is also depressed is going to put more of a burden on family members to make sure they take their medications.” ▪



