CMS Proposes 1.5 Percent Increase For 2005 Medicare Physician Fees
A new physician fee schedule implementing an across-the-board increase of 1.5 percent in 2005 for physicians participating in the Medicare program has been proposed by the Centers for Medicare and Medicaid Services (CMS).
The fee schedule was issued as part of a proposed rule implementing provisions of the Medicare Modernization Act of 2003. It was published in the August 5 Federal Register. Comments will be accepted until September 24. CMS plans to publish the final rule by November 1, with an effective date of January 1, 2005.
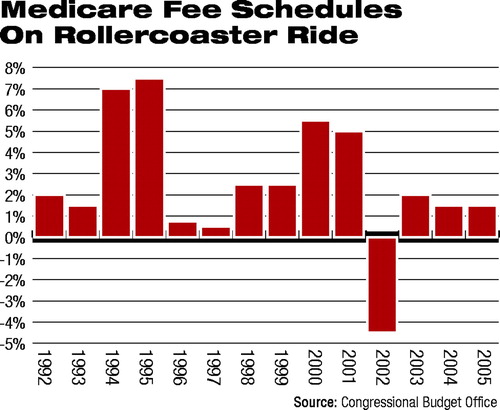
The proposed 1.5 percent increase replaces a decrease of 3.7 percent that had been previously projected. The AMA, along with APA and other groups, vigorously opposed the projected decrease and lobbied for an increase.
However, the 1.5 increase represents the average across all specialties. Some specialties may experience an even higher increase, while some may experience a lower increase or even a decrease in payments. At press time, analysis of how the proposed fee schedule could affect psychiatry was under way by APA's Department of Government Relations and Office of Healthcare Systems and Financing; details will appear in Psychiatric News as soon as they become available.
Chester Schmidt, M.D., chair of APA's Committee on RBRVS, Codes, and Reimbursement, noted that despite the across-the-board increase for 2005, decreases are projected by CMS beginning in 2006.
“We hope that psychiatrists will benefit from the 1.5 percent across-the-board increase and are waiting for an analysis of how the fee schedule will affect the profession,” said Schmidt. “But along with the rest of medicine, we remain very concerned about projected cuts in coming years.”
Edward Gordon, M.D., chair of APA's Medicare Advisory Committee, noted that in a “zero sum” budget, any increase in services means that money will have to be taken from somewhere else.
And overriding payment issues for psychiatry is the discriminatory 50 percent copayment for outpatient mental health services. “A lot of psychiatrists simply won't treat Medicare patients on an outpatient basis,” he said.
The AMA hailed the proposed increase while continuing to argue that the entire formula by which physician payments are calculated should be scrapped.
“This rule puts in place the 1.5 percent increase in Medicare physician payments from the [new] Medicare law,” said J. James Rohack, M.D., chair of the AMA's board of trustees. “Efforts by Congress and the Bush administration prevented an access-to-care crisis for patients this year and next by halting a 4.5 percent cut in Medicare payments this year and a 3.7 percent cut in 2005.
“The narrowly averted 2004 and 2005 cuts—and the upcoming cuts forecast for 2006 through 2012—are an alarm bell for America's Medicare patients and their physicians that the flawed payment formula must be replaced,” said Rohack. “There is much work to be done to ensure that all our Medicare patients have access to care in the future. The AMA will continue its work with Congress and the administration to reform the flawed Medicare payment formula.”
Total Medicare spending for more than 875,000 physicians and other health care professionals will increase by more than 4 percent, from a projected $52.7 billion in 2004 to a projected $55 billion in 2005, according to CMS.
The CMS's proposed rule also includes these provisions:
New incentive payments to doctors practicing in physician-scarcity areas. These payments of 5 percent would be made to both primary care and specialty physicians furnishing services to beneficiaries in the areas with the lowest 20 percent of physician-to-beneficiary ratios. | |||||
Authorization of psychologists to receive payment for both administering diagnostic psychological tests and for supervising the administration of these tests. | |||||
New coverage for a one-time evaluation and counseling from a physician employed by a hospice to determine appropriate end-of-life services for terminally ill beneficiaries. | |||||
The proposed fee schedule is posted at<http://a257.g.akamaitech.net/7/257/2422/06jun20041800/edocket.access.gpo.gov/2004/04-17312.htm>.▪



