States Seek Solutions To Public Health Crisis
At the annual Health Leaders Seminar of the National Conference of State Legislatures (NCSL) last month in Washington, D.C., speakers presented a complicated picture of the impact of state budget cuts on Medicaid.
One clear finding is that those who provide medical services to Medicaid patients have seen their already low rates of reimbursement diminish even more.
Victoria Wachino, associate director of the Kaiser Commission on Medicaid and the Uninsured, said that to control costs states have relied primarily on reducing or freezing provider payments and controlling spending on prescription drugs.
Jane Woods, Virginia’s superintendent of Health and Human Services, reported that the state reduced payments to hospitals and that physicians had not had an increase in reimbursement rates for 14 years. She added, “We have truly, truly hurt our providers in case anyone missed that point. I would caution every state, because at some point you are denying access when you do that.”
Speakers emphasized the importance of the “dual eligibles” (beneficiaries who are eligible for both Medicare and Medicaid) in efforts to restrain Medicaid costs.
Wachino reported that about 42 percent of all Medicaid spending goes to people who are enrolled in both programs. About 6 percent of all Medicaid spending goes to prescription drug coverage for them.
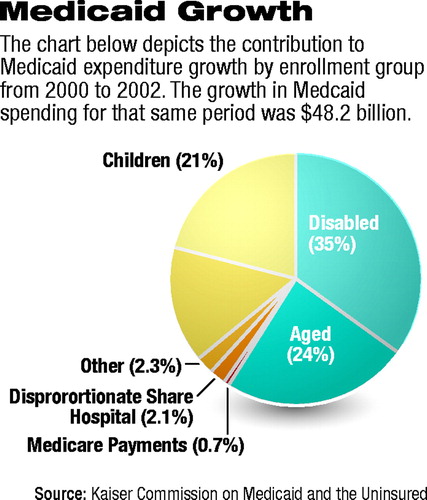 The categories “disabled” and “aged” were responsible for 60 percent of the Medicaid expenditure growth from 2000 to 2002 (see chart).
The categories “disabled” and “aged” were responsible for 60 percent of the Medicaid expenditure growth from 2000 to 2002 (see chart).
The recent Medicare legislation includes a provision for the federal government to pick up some costs for prescription drugs for this population (Original article: see page 1).
Wachino noted that when the prescription drug benefit program becomes operational in 2006, states will have considerable added administrative responsibility and costs because they will be required to help the federal government determine eligibility for a low-income subsidy for the Medicare drug benefit.
Chuck Milligan, a principal with the Lewin Group, told attendees that the Bush administration will revive efforts to turn Medicaid into a modified block-grant program.
Early in 2003 Tommy Thompson, secretary of Health and Human Services, announced a plan that would have offered states more flexibility in terms of services they would be required to offer to some populations covered by Medicaid.
The plan was denounced by APA and other mental health advocacy organizations.
Then APA president Paul Appelbaum, M.D., said, “Rather than using Medicaid as a base on which to build a program that would cover all Americans, the administration is moving in the wrong direction, providing incentives to the states that ultimately will result in reduced coverage. Indigent people with mental illness likely will be hurt most.”
The administration withdrew the plan when the National Governors Association refused to support it.
According to Milligan, the Centers for Medicare and Medicaid Services (CMS) recently has been reluctant to approve states’ requests for Medicaid waivers, after initially encouraging their use. He said, “[S]omebody at CMS said at a meeting a few months ago [that] it somewhat undermines the arguments that you need legislative block grants if you get the flexibility through waivers.”
Woods said that Virginia state officials had worked with CMS for two years to get a waiver that would have allowed more home-based care for older people and had recently been turned down.
“CMS is now saying don’t even bother to submit these waiver amendments. We will not approve them,” she told the group.
Milligan described positive outcomes of the increased fiscal constraints. As part of an effort to uncover fraud and abuse, one state identifies patients who receive more than 10 medications. As result, cases of “bad prescribing” have been identified.
Some states are implementing assertive community treatment programs.
He urged the legislators to make structural changes that are appropriate and sustainable over the long haul.
In the short term, several legislators reported a “kind of civil war” between advocates for spending on education and on health care.
A transcript of the meeting, “Medicaid and Budgets: From Impasse to Impact,” is posted online at www.kaisernetwork.org/health_cast/uploaded_files/120903_ncsl_medicaid.pdf. ▪



