Psychiatrists to Get Assistance Navigating New Drug Benefit
APA's Office of Healthcare Systems and Financing (OHSF) hosted a meeting of district branch and state association (DB/SA) executives at APA headquarters in Arlington, Va., last month as part of its effort to ensure that psychiatrists have resources to help their patients transition into the new Medicare Part D drug benefit that begins on January 1, 2006.
The meeting debuted a draft set of tools, identified key issues still needing to be addressed, and identified what needs to be done next as the start of the drug-benefit program draws nearer.
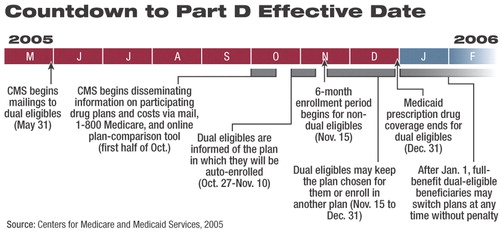
The transition to Part D may be the largest rollout of a prescription-drug benefit in history, and the complexity of its administration will burden both patients and their physicians. For example, patients are bound to have numerous questions and concerns as they attempt to digest complicated information and select the optimum prescription drug plan (PDP) for them, especially because they won't have much time to decide on a plan before the program begins (see chart).
The transition to Part D is expected to be problematic for many patients, including the estimated 6.4 million dual-eligible patients whose prescription drug coverage will be moved from Medicaid to Medicare Part D on January 1, 2006.
Since late 2003, APA has been working with a steadily expanding coalition to address the many problems that patients are expected to face as they make the transition to the new benefit. The coalition now includes the National Alliance for the Mentally Ill, National Mental Health Association, National Council for Community Behavioral Health, Treatment Effectiveness Now Project, American Association of Community Psychiatrists, National Association of State Mental Health Program Directors, and Substance Abuse and Mental Health Services Administration.
The coalition approach, noted OHSF Director Irvin Muszynski, J.D., has worked well for APA and helped to “bring all the partners onto the same page. The resulting collective force of will has been effective.”
The coalition's efforts, for example, likely played a significant role in a June decision by the federal Centers for Medicare and Medicaid Services (CMS) to mandate that participating PDPs cover “all or substantially all” antidepressant and antipsychotic medications (Psychiatric News, July 15).
As patients sign up for a PDP, the coalition would like to have the capacity to collect data on problems encountered by patients on a real-time basis and provide that data directly to CMS. However, at this time, such a complex monitoring system is just a proposal, and funding for such a project has not yet been completely secured.
Muszynski chaired the August meeting, which included representatives of several coalition members. About 10 DB/SA executives attended the meeting, while 10 additional executives participated via conference call.
“From the start,” Muszynski said to the DB/SA executives,“ our central question has been, What do physicians really need to know about Part D as we head through these final months [leading up to the program's start]? We need to know what you need.”
All Part D benefits will be administered through geographic regions defined by CMS. Each region must have at least two PDPs from which patients can choose to administer their drug benefits. However, because CMS regulations allow PDPs to develop their own drug formularies (within limits specified in guidelines), coverage of psychiatric medications may differ among PDPs. How can patients ensure they select the plan that is best and most cost-effective for them?
“It would help physicians tremendously, for example, to be able to determine—with as little time and effort as possible—whether a particular PDP that a patient has been assigned to under Part D is appropriate for that patient or not,” Muzysnki told Psychiatric News.“ The coalition members are working together to have common materials developed and hosted on a shared Web site that would help practitioners answer questions such as that.”
DB/SA executives identified key issues with which they are concerned, including the coverage-determination process and supporting patients in the process of applying for exceptions or appeals when determinations become denials. Many had concerns about utilization management techniques that PDPs may use, such as limitations on dosage, number of doses, or route of dosing on some medications.
Identifying state-related issues was another concern of the DB/SA executives. Regulations, such as those that address whether a state will pay for medications not covered by Part D—benzodiazepines, for example—vary by state. Moreover, one state may be covered by more than one Medicare Part D geographic region.
Over all, the DB/SA executives recommended that the materials developed be narrowly targeted to address specific populations of patients and their needs with respect to Part D coverage. For example, some patients qualify for Part D coverage through Medicare because of age, while others qualify through Medicaid because of disability and low income.
By the end of the day-long meeting, APA staff, coalition members, and DB/SA executives had identified the need for advocacy plans for individual states, concise information on each PDP's drug formulary with respect to psychiatric medications, a “fast facts” set of resources on key issues, and a set of “frequently asked questions.”
When finalized, materials will be posted in the Members Corner area of APA's Web site at<www.psych.org/members/index.cfm?>.▪



