Med Check
Regulatory and Legal Briefs
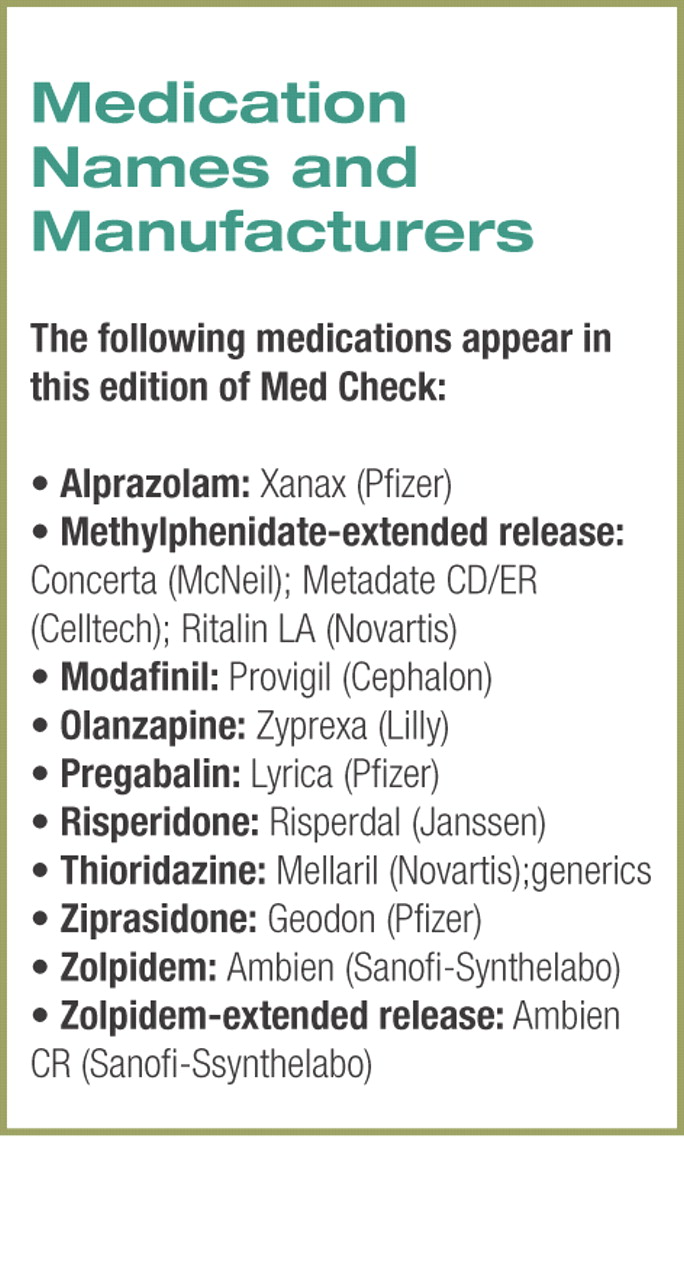
• Zolpidem–extended release was approved by the U.S. Food and Drug Administration (FDA) last month for the treatment of insomnia. The non-narcotic, nonbenzodiazepine hypnotic is a longer-acting version of zolpidem, which has been on the U.S. market since 1992. The new two-layer formulation has an outer layer that dissolves quickly and a second layer that dissolves slowly over several hours.
Like the immediate-release version, the new formulation will be a Schedule IV controlled substance and is recommended for the short-term (seven to 10 days) treatment of insomnia.
In clinical trials, the extended-release formula was not only effective at reducing time to sleep onset but also maintaining sleep throughout the night. The most frequently observed side effects during clinical trials were drowsiness, dizziness, and diarrhea.
Zolpidem–extended release will be available in a 12.5 mg tablet for adults and a 6.25 mg tablet recommended for elderly patients.
• Health Canada ended distribution of thioridazine in Canada as of September 30. Pharmacies can continue to dispense stock on hand, giving patients some time to consult with their health care providers on switching to another medication.
The regulator said the suspension of marketing approval was based on“ concerns about the use of the medication and rare occurrences of heart rhythm changes that could be life threatening.” Health Canada said that information submitted by the manufacturer “has failed to demonstrate that the benefits outweigh the risks” associated with the medication.
Research Briefs
• Pregabalin is significantly more efficacious than placebo for the treatment of psychic and somatic symptoms of generalized anxiety disorder and is well tolerated. A double-blind, placebo-controlled, active comparator trial compared pregabalin at three dosages (300 mg/day, 450 mg/day, and 600 mg/day) with alprazolam (1.5 mg/day) and placebo in more than 450 patients for four weeks.
The Hamilton Anxiety Rating Scale scores of subjects in the three pregabalin groups and the alprazolam group were statistically significantly reduced.
Both pregabalin and alprazolam were significantly associated with somnolence and dizziness. In addition, pregabalin was significantly associated with dry mouth, nausea, and blurred vision. The study was funded by Pfizer.
Arch Gen Psychiatry 2005; 62:1022-1030
• Ziprasidone and olanzapine have similar long-term efficacy but differ significantly in their tolerability profiles. A group of 126 patients from a six-week acute study of the two drugs was followed for an additional six months under double-blind conditions. The two drugs were associated with comparable improvements in patient scores on the Brief Psychiatric Rating Scale and Clinical Global Impression–Severity of Illness scale.
Compared with ziprasidone, olanzapine was associated with significant increases in weight and body mass index, as well as increases in total cholesterol, low-density lipoprotein cholesterol, and fasting insulin. Neither drug was associated with significant increases in electrocardiogram QTc intervals. The study was funded by Pfizer. Am J Psychiatry 2005; 162:1535-1538
• Neither risperidone nor olanzapine was significantly better than placebo for the treatment of patients with behavioral and psychotic symptoms of dementia (BPSD). A double-blind, placebo-controlled comparator trial evaluated the two drugs in nearly 500 patients with moderate to severe BPSD over 10 weeks. Dosage was flexible, ranging from 2.5 mg/day to 10 mg/day of olanzapine and 0.5 mg/day to 2 mg/day of risperidone. Patients' BPSD were rated using the Neuropsychiatric Inventory and the Clinical Global Impressions–Severity of Psychosis scale.
Subjects in all three treatment groups, including placebo, improved in most measures of functioning with no statistically significant differences between groups. Discontinuation of drug due to adverse effects was highest in the olanzapine group at 16.2 percent, compared with 8.7 percent in the risperidone group and 3.2 percent in the placebo group. Extrapyramidal symptoms were most frequently observed in patients taking risperidone. Prolactin levels were elevated in 78 percent of those taking risperidone compared with 16.7 percent of those taking olanzapine and 5 percent of those taking placebo.
Weight gain was greatest in those taking olanzapine; however, there was no statistical difference between the three groups for weight gain.
Eli Lilly and Co. funded the study. Am J Geriatr Psychiatry 2005; 13:722-730
• Atypical antipsychotics are just as likely as older, typical antipsychotics to cause tardive dyskinesia and other movement disorders, including parkinsonism, in elderly patients with dementia. Two retrospective cohort studies followed nearly 22,000 elderly residents of Ontario who had dementia and had recently been started on an antipsychotic drug. Atypicals were prescribed to 9,790 patients, while 12,045 patients were prescribed typical antipsychotics.
There was no statistically significant difference in the number of patients who developed tardive dyskinesia on atypical drugs compared with typical drugs. In addition, patients taking higher doses of the atypical drugs had similar incidences of parkinsonism associated with medication therapy as patients taking lower-potency typical drugs. However, those taking low to moderate doses of atypical agents were 30 percent less likely to develop parkinsonism. The study was funded by grants from the Canadian Institutes for Health Research.
Arch Intern Med 2005; 165:1882-1888; J Am Geriatr Soc 2005; 53:1374-1379
Industry Briefs
• Modafanil is expected to receive final FDA approval soon for the treatment of attention-deficit/hyperactivity disorder. The drug will be jointly promoted by McNeil Consumer and Specialty Pharmaceuticals and Cephalon Inc. More than 300 McNeil representatives who currently sell the company's methylphenidate (extended release) will promote modafinil to pediatric specialists, while about 400 Cephalon representatives will promote the drug to psychiatrists, neurologists, and primary care physicians.
Modafinil is approved for the treatment of excessive sleepiness associated with narcolepsy, obstructive sleep apnea/hypopnea syndrome, and shift-work sleep disorder. The most frequently observed adverse effects associated with modafinil are headache, nausea, nervousness, stuffy nose, diarrhea, anxiety, difficulty sleeping, and dizziness.▪