Treating Depression Boosts Immune Response to HIV
Depression can not just weaken the body's immune system, but encourage disease progression in HIV-infected individuals, research conducted by Dwight Evans, M.D., chair of psychiatry at the University of Pennsylvania, and others has suggested.
And now Evans and his colleagues report a new finding that also points to a link between depression and immunity in HIV-infected individuals. Depression in HIV-positive persons not only appears to impair certain immune cells that may be crucial to fighting HIV, but if the depression resolves, the damaged immune cells seem to rebound.
In this study, which was published in the November American Journal of Psychiatry, Evans and his group assessed 57 HIV-positive women at baseline and then a year later for depression. They also evaluated the women at baseline and again after one year for activity of a particular type of immune cell—the natural killer cell—which appears effective in fighting HIV infection. They then looked for associations between changes in depression status and natural killer cell activity over time.
Of the 57 subjects, 43 did not meet criteria for a major depression at the start of the study and remained depression-free throughout, 11 were diagnosed with major depression at the start of the study, but not by the end of it, and three did not have major depression at the start, yet did by the study's end.
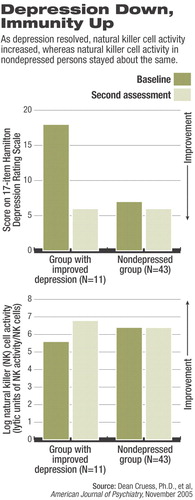
The 43 subjects who were not depressed throughout the study did not show any significant change in natural killer cell activity during that period.
In contrast, the 11 subjects who were depressed at the start of the study, but whose depression had resolved by the end of it showed a significant increase in natural killer cell activity during that period.
As for the three subjects who were not depressed at the start of the study, yet were at the end, two showed some reduction in natural killer cell activity during that period.
Depression improvement in all subjects was significantly linked with an increase in natural killer cell activity even when possibly confounding factors such as HIV viral load, HIV medication status, and antidepressant medication status were considered.
Remaining to be demonstrated, however, is whether successful treatment of depression also spells actual retreat of HIV infection in the body. “In newly funded NIMH studies,” Evans told Psychiatric News,“ we are currently assessing the effects of potential antidepressant treatments on the relationship of depression, immunity, and HIV disease progression with a focus on the underlying mechanisms.”
The study was financed by the National Institute of Mental Health.
“Association of Resolution of Major Depression With Increased Natural Killer Cell Activity Among HIV-Seropositive Women” is posted at<http://ajp.psychiatryonline.org> under the November issue.▪