Beneficiaries Can Delay Fall Into Medicare's `Donut Hole'
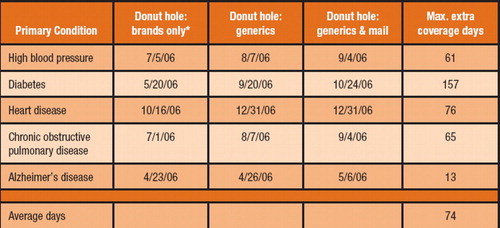
Medicare patients with Alzheimer's disease who use generics and mail-service pharmacies can potentially add an additional 13 days to their Medicare Part D coverage and delay entry into the Medicare Part D coverage gap, or “donut hole.”
That was one finding from an analysis of the effect of generic-drug use on prescription drug costs for patients with five common conditions. The analysis was performed by the Pharmaceutical Care Management Association (PCMA).
PCMA is the national association representing the nation's pharmacy benefit managers.
The donut hole refers to the gap in coverage between $2,250 and $3,600 in yearly expenses for prescription drugs. Under the Medicare Modernization Act of 2003, a beneficiary may not be covered for prescription drug costs beyond $2,250 in one year; once costs reach $3,600, coverage begins again.
Not all Medicare Part D prescription drug plans have a donut hole, however. The Centers for Medicare and Medicaid Services reported in August that 28 percent of individuals enrolled in Medicare Part D are in plans that have a coverage gap. Thus, the majority of Part D beneficiaries are not subject to the donut hole.
For patients with Alzheimer's, the total out-of-pocket savings by using generics and mail-order services would be relatively small at $38, or only 1 percent (see table). Part of the reason for the relatively small savings in this category is that there are very few generic alternatives, according to PCMA
But PCMA found that overall, increased use of generic drugs and mail-service pharmacies by Medicare beneficiaries has the potential to delay entry into the Medicare Part D coverage gap by an average of 74 days.
“Regrettably, too many beneficiaries are not taking full advantage of the cost-saving tools within their Medicare drug plans,” said PCMA President Mark Merritt in a statement accompanying release of the analysis.“ All stakeholders need to work together to make beneficiaries better aware of how to maximize their Medicare prescription drug coverage, including increased use of generics and mail-service pharmacies.”
In the analysis, PCMA assembled five patient profiles using both brand-name and generic drugs to treat five primary conditions and assorted related conditions. The conditions were high-blood pressure, diabetes, heart disease, chronic obstructive pulmonary disease, and Alzheimer's disease.
PCMA examined four national Medicare prescription drug plans that provide coverage to more than 50 percent of Medicare's prescription drug plan beneficiaries.
On average, beneficiaries can save in total about 38 percent—or more than $1,200 in 2006—in out-of-pocket costs through the increased use of generic drugs and mail-service pharmacies.
Additional days of coverage and costs saved for the other four conditions, according to analysis, are as follows:
High-blood pressure. Sixty-one additional days of Part D drug coverage, with total out-of-pocket savings of $1,226, or about 36 percent. | |||||
Diabetes and other related conditions. An additional 157 days of Part D drug coverage, with total out-of-pocket savings of $2,081, or about 57 percent. | |||||
Heart disease and other related conditions. An additional 76 days of Part D drug coverage, with total out-of-pocket savings of $1,221, or about 57 percent. For this profile, patients would avoid entering the donut hole altogether, according PCMA. | |||||
Chronic obstructive pulmonary disease and other related conditions. An additional 65 days of Part D drug coverage, with total out-of-pocket savings of $1,504, or about 42 percent. | |||||
A report of the PCMA analysis and methodology is posted at<www.pcmanet.org/newsroom/index.htm>.▪



