States Try Several Strategies to Expand Health Coverage
Proposals in several states to expand the number of residents with health insurance through government-sponsored programs are also mandating that mental health coverage be part of the package.
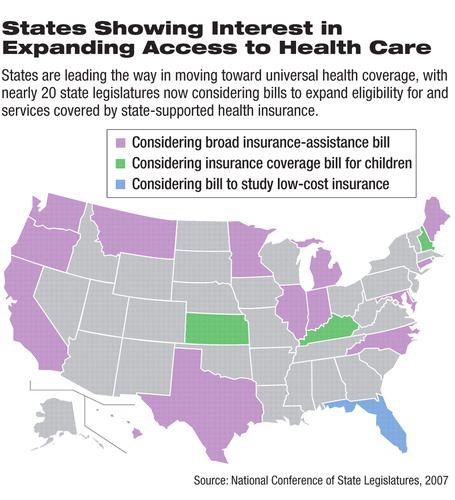
Massachusetts and Vermont were in the vanguard, passing laws in 2006 to achieve near universal coverage and to control cost and quality of health care. At least 10 other states are considering comprehensive health insurance legislation or have administrative proposals under review, and several more have established committees to study health care reform.
The state efforts have many features in common, and most include market reforms, subsidized health insurance, assessments against employers who don't offer health insurance, wellness initiatives, disease management, Medicaid expansions, and qualit y-improvement components. Most plans also include mental health coverage.
“Mental health has come up a lot in discussion of our plan, and it is a critical component,” said Krista Donahue, chief of policy in the Illinois Department of Healthcare and Family Services, about the governor's proposed health coverage expansion.
Illinois Gov. Rod Blagojevich's (D) proposal, known as Illinois Covered, would provide affordable health insurance to the state's 1.4 million uninsured adults. The proposal, working its way through the state legislature, requires all private insurers in Illinois to provide an affordable, comprehensive, state-subsidized insurance option for employees of small businesses and other uninsured individuals. Other components include granting an insurance-premium rebate, allowing parents to include offspring up to age 30 on their insurance, and expanding eligibility of parents who get coverage through the state to those earning up to 400 percent of the federal poverty income level.
The proposal has several mental health components, including a requirement that the private-insurance option for small employers and individuals cover“ medically necessary” mental health services. These are defined to include services to “restore, maintain, or prevent deterioration of an enrollee's condition.” The privately offered option would have to accept individuals regardless of previous or current use of mental health services, and health status could no longer determine costs of that coverage.
Mental health benefits would cover assessment, emergency care, prescription drugs, inpatient and outpatient hospital care, physician services, and mental health clinic services such as counseling, and group therapy.
Advocates of the health care proposal, which requires no federal funding, hope the Illinois legislature will pass the plan later this year or in early 2008.
Pennsylvania Plans Expansion
Less-comprehensive mental healt h changes are part of health care expansion legislation in Pennsylvania. The Prescription for Pennsylvania proposal, advocated by Gov. Edward Rendell (D), would make affordable basic health care coverage available to small-business employees through the private insurance market. The program would emphasize pay for performance and encourage“ wellness” and preventive care and chronic-disease management.
In addition, the program would require all insurers offering small-group and individual plans to provide a standard plan that includes basic benefits. Mental health coverage, including that for substance abuse, would not be required in the basic plan, but insurers would have to make such coverage available as an option at additional cost. Insurers would be prohibited from excluding children with behavioral health needs from coverage.
Donna Cooper, secretary of the Pennsylvania Governor's Office of Policy and Planning, told Psychiatric News at a Washington, D.C., briefing on the plan that the program does not place much emphasis on mental health care because there appeared to be little demand for that from health advocates in the state.
“We haven't had a lot of lobbying on mental health issues when putting together this plan,” said Cooper.
Deb Shoemaker, executive director of the Pennsylvania Psychiatric Society (PPS), disputed that lobbying claim in an interview with Psychiatric News, noting that PPS members have testified before several legislative committees and lobbied their local representatives.
The plan also anticipates major cost savings through an expanded role for allied health practitioners, including advanced nurse practitioners, midwives, physician assistants, pharmacists, and other licensed health care providers. The plan would provide additional authority to nurses to diagnose mental illnesses and prescribe medications, according to Cooper.
PPS representatives have testified against the scope-of-practice expansion proposed for clinical nurse specialists, certified nurse practitioners, and nurse midwives as part of the health care overhaul. The expanded authority sought for these nurses would allow some to commit patients involuntarily, prescribe psychotropic drugs, and diagnose mental illness.
“Without the extensive training that psychiatrists have, these allied health professionals are limited in what they can do for the public,” said PPS's Shoemaker.
Rendell hopes that the insurance expansion will be in place by January 2008, Cooper said.
Potential Obstacles Await
Critics of the various state health care proposals maintain that some of their provisions are illegal under federal law. The 1974 Employee Retirement Income Security Act (ERISA) prohibits states from requiring employers to set aside health care paycheck deductions, for example. State officials said they are getting around ERISA prohibitions on state insurance-plan mandates, in part, by creating a tax on insurers that is refundable if they offer specific types of plans.
Donahue said supporters expect the Illinois program to withstand ERISA legal challenges, although problems could arise if employers offer only limited coverage, because state officials don't want to force them to offer more.
Members of Congress have begun to discuss ERISA changes that would allow more state health care coverage efforts, and the National Governors Association is expected to announce its support for a number of ERISA changes this summer.
Another sticking point for states is how to fund the plans. Illinois is reconsidering a proposed tax on gross receipts, due to stiff political opposition. Pennsylvania plans to use previously appropriated but unused Medicaid funds to pay for part of the expansion.
Among the states that already have approved health coverage overhauls, Massachusetts uses low-cost insurance plans paid for by enrollees, businesses, and government subsidies. Vermont funds its program through a Medicaid waiver, state funds, a tobacco tax, and business assessments.
Most states attempting to implement comprehensive health care programs aim to build on the Medicaid and State Children's Health Insurance Program (SCHIP) approaches, which cover the poorest first and expand eligibility up the“ economic ladder,” according to Joy Johnson Wilson, health policy director and federal affairs counsel for the National Conference of State Legislatures.
The challenge for states undertaking such reforms has been finding ways to keep employers participating in the increasingly expensive employee insurance market. In recent years, however, states have become more willing to take on insurance-industry and business-community opposition because of the urgency to remedy the lack of insurance coverage among so many state residents.
Enrique Martinez-Vidal, acting director of state coverage initiatives at the Robert Wood Johnson Foundation, said he expects more states to undertake increasingly ambitious health care overhauls due to federal inaction, growing support for health care initiatives in state legislatures, and a generally positive economic outlook at the state level.
“However, it is unrealistic to think that all states have the financial ability to undertake such comprehensive reforms without strong federal support,” he added.
Information on the Illinois proposal is posted at<www.illinoiscovered.com/>. Information on the Pennsylvania proposal is posted at<www.gohcr.state.pa.us/prescription-for-pennsylvania/PlainEnglishLegislation.pdf>.▪



