States Vary in Commitment to Their Uninsured Residents
Economic factors have been a key ingredient in the rapid growth of the number of uninsured adults in recent years, according to a new scorecard of statewide health factors. The declining levels of insurance coverage were linked to poorer health among the populations of many states.
The good news is that expanded federal and state spending on children through Medicaid and the State Children's Health Insurance Program have led to better insurance coverage and improved health among children in many states in recent years.
States in the Northeast and upper Midwest had more effective policies and programs to promote health among users of public and private health care, according to the report “Aiming Higher: A State Scorecard on Health Care System Performance,” by the Rutgers University Center for State Health Policy and the Commonwealth Fund.
States with the best overall health care outcomes consistently outperformed the weaker states in every specific health care category measured, such as high quality and safety. These statewide trends suggested to the authors that policies and programs that encouraged better health care were the cause. The scorecard used a variety of data sources to measure health care quality, access, crisis-related hospital use and costs, and healthy lives. The measures were designed to identify which states are the closest to a “high performance health system” that is able to help residents achieve lives that are as long and healthy as possible.
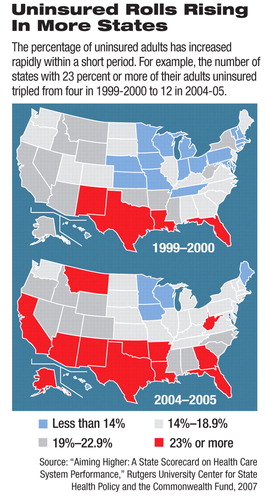
The core finding, the researchers said, was the crucial role played by changes in health insurance coverage, which reduced health care access. The number of states with 23 percent or more of their adults uninsured tripled from four in 1999-2000 to 12 in 2004-05. In the same period, the number of states with less than 14 percent of adults uninsured dwindled as employer coverage became less affordable and costs outstripped wages.
“One of the themes we see running throughout the scorecard is this close correlation of access and quality,” said Cathy Schoen, senior vice president at the Commonwealth Fund and one of the report's authors, during a June press briefing on the scorecard. “States that do well on access are also doing well on quality.”
Economy Often Key Factor
The problems with access are linked to economic trends in many states. One state with declining health measures, Oklahoma, experienced a series of economic setbacks in the last 20 years as its core oil industry hit hard times. That state is one of a growing number with at least 23 percent of adults aged 18 to 64 who are uninsured.
“We have one of the highest rates of uninsurance in the country,” said Peter Budetti, M.D., a professor at the University of Oklahoma College of Public Health.
Age-adjusted mortality rates in Oklahoma used to be very close to the national mortality rates, but they suddenly separated a decade ago, he said, when his state's rate exceeded national norms.
Even states that did better in the scorecard experienced declines in recent years. Chris Koller, Rhode Island's health insurance commissioner, said a variety of factors contributed to the rise in the number of uninsured adults in his state.
Koller said 45,000 state residents lost insurance from 1999-2000 to 2004-05 because employers tightened eligibility to exclude part-time workers. Companies took this action to control the rising costs of insuring their full-time workers.
Mary Wakefield, associate dean for rural health at the University of North Dakota School of Medicine, said good scorecard results for her state were linked to several factors, including a higher-than-average ratio of primary care providers to population. Research studies, she said, have identified primary care as the key to managing chronic and expensive-to-treat conditions such as diabetes and asthma.
“States that rely more on primary care to manage chronic illness tend to have lower Medicare spending and use fewer hospital beds,” she said.
Schoen noted that the scorecard did not find a “systematic relationship” between health care costs and quality. The report identified several instances of states that had widely available, high-quality care that were spending less than states where quality of care lagged.
Solutions Differ
Highlighting some state efforts to improve the overall health measures assessed in the scorecard report, Koller noted that Rhode Island has launched an effort to fund expanded disease-prevention efforts and will seek more federal assistance to augment that effort.
Oklahoma has started an insurance-subsidy program for employees of small businesses to compensate for the declining number of such businesses offering health insurance. It also is using increased cigarette taxes to fund health care programs and a healthy-living initiative to raise its residents' awareness of health-related issues.
Increased use of health-information technology and telemedicine, Wakefield said, should improve statewide health care outcomes, especially in states with large rural areas. The most promising approaches will increase coordination of the health care provided, such as expanded use of “medical homes,” which assign one clinician to coordinate all of a patient's health care needs.
“I would encourage health staff to think about this, to think about filtering every policy, piece of legislation, program that you are evaluating through a prism that helps you to distinguish whether the policy or piece of legislation you are looking at will further fragment or splinter health care delivery and payment policy, or whether [it] could help to build system-ness, cohesion, and coordination into health care,” she said.
“Aiming Higher: A State Scorecard on Health Care System Performance” is posted at<http://allhealth.org/briefing_detail.asp?bi=108>.▪



