Obstacles Hinder Search for Mental Illness Genes
More than a thousand geneticists from dozens of countries gathered in New York in October to focus on a daunting challenge—identifying genes underlying various psychiatric illnesses. It was the 15th World Congress on Psychiatric Genetics, cosponsored by New York University and the International Society of Psychiatric Genetics (see Original article: Psychiatric gene Researchers Urged to Pool Their Samples for additional coverage of the congress).
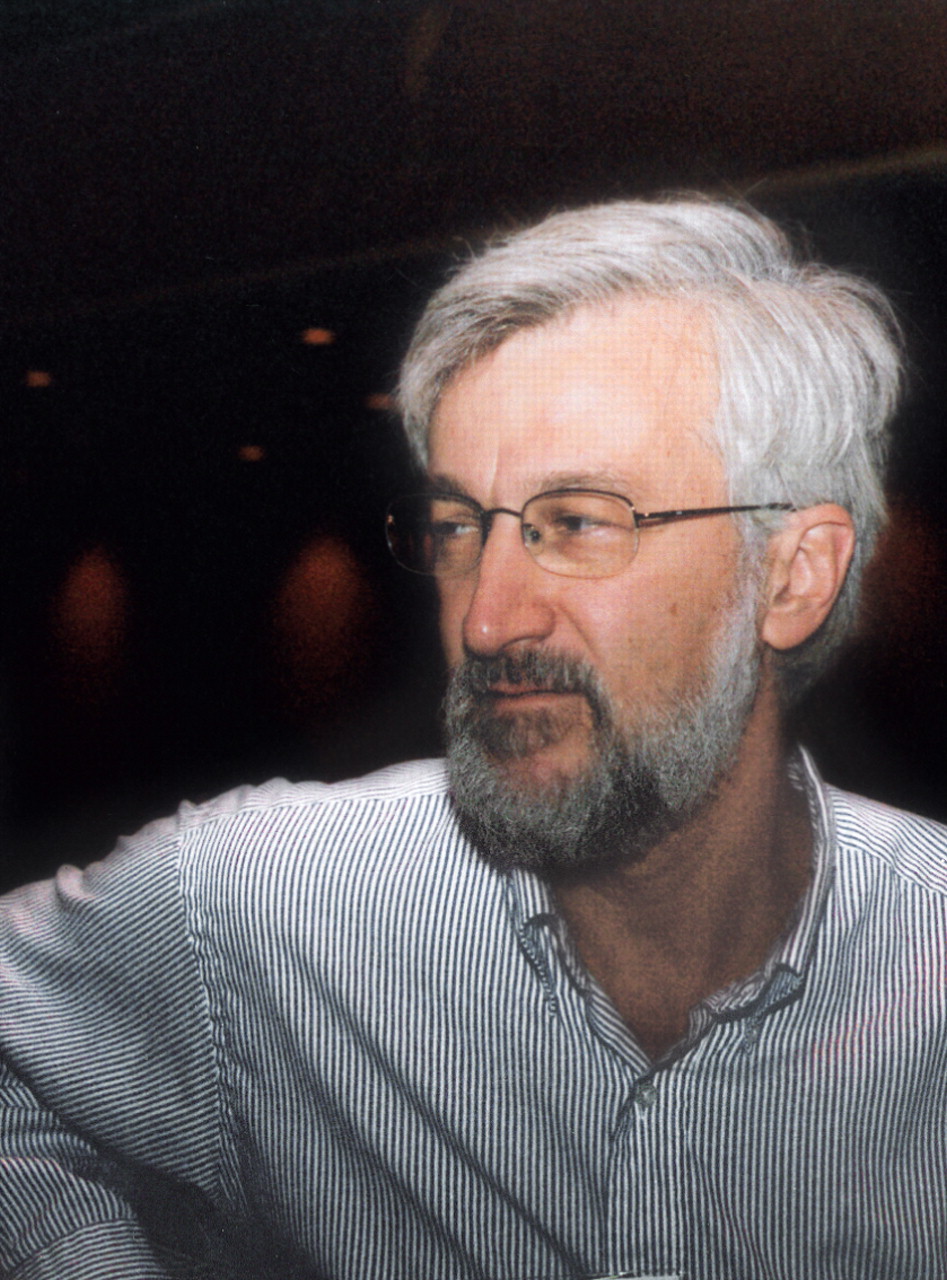
Launching the congress was James Watson, Ph.D., who shared a Nobel Prize in Medicine in 1962 for the discovery of the structure of DNA.
During his talk, Watson noted a great irony considering the theme of the congress—he has a son with schizophrenia. “If you don't have a child with schizophrenia, you don't know what it is like,” he said. Thus his family is one of many throughout the world who might profit from the identification of genes that contribute to psychiatric illness. Yet it is unfortunately going to be a while before they reap such benefits, he and other speakers indicated.
Challenges Abound
The challenges facing geneticists as they go about trying to definitively identify psychiatric genes are certainly formidable.
One of them is difficulty in replicating their findings, which in turn may be due to using too few subjects in a study or using samples that are too heterogeneous, said Markus Noethen, Ph.D., of the Life and Brain Center at the University of Bonn in Germany.
Another hurdle, speakers indicated, is that a plethora of genes with miniscule effects, not one dominant gene inherited in a Mendelian fashion, seems to underlie psychiatric disorders. For example, even though autism appears to be “overwhelmingly genetic,” the evidence implies that it is due to a number of genes, and “we don't really know the real numbers,” said Joseph Buxbaum Ph.D., a professor of psychiatry at Mt. Sinai School of Medicine.
Yet another obstacle concerns the sequencing of the human genome. It was completed in 2003 and has proven to be a great boon in the search for genes that contribute to various illnesses. But also thanks to the sequencing of the human genome, geneticists are now faced with such a vast amount of genetic information that “it is really quite daunting,” James Kennedy, M.D., a professor of psychiatry at the University of Toronto, admitted.
And still another difficulty is integrating findings from the current popular method of genetic analysis—genome-wide association studies—with those obtained from an earlier method of looking for psychiatric genes—linkage analysis, Pamela Sklar, M.D., Ph.D., an associate professor of psychiatry at Harvard Medical School, pointed out.
But perhaps most troubling is what Patrick Sullivan, M.D., a professor of psychiatry and genetics at the University of North Carolina, reported: candidate gene studies can produce many false positives. In fact, only a minority of association studies in biomedicine have withstood replication over time, he pointed out. To which a geneticist in the audience responded:“ Nice talk! Discouraging, though.”
These challenges, not surprisingly, have led to some disappointments.

Karola Rehnstrom of the University of Helsinki in Finland: “Autism spectrum disorders have a strong genetic component, but only a few genetic causes have been identified so far.”
Credit: Joan Arehart-Treichel
Studies have suggested that there might be bipolar disorder genes on a number of chromosomes, “but none of the genes identified to date has been accepted by the scientific community,” Noethen said.
“And if you think that the genes contributing to bipolar disorder are complicated, it could be that schizophrenia genes [are even more so],” Kennedy added. He and his colleagues had hoped that they could “parse out” the genes for bipolar disorder and schizophrenia, yet their efforts have been “completely unsuccessful,” he said.
Unfortunately, Karola Rehnstrom, a doctoral candidate in medical genetics at the University of Helsinski in Finland, reported that the autism-gene results that she and her colleagues have obtained with genome-wide association studies do not coincide with the results that they obtained with linkage-analysis studies.
“The state of autism [gene research] is the state of psychiatric genetics,” lamented Buxbaum. “We are not as far as we would like to be.”
Some Progress Made
Nonetheless, progress has been made toward pinpointing psychiatric genes, speakers indicated.
Several genes that contribute to Alzheimer's disease, notably the APOEe4 variant, have been identified (Psychiatric News, April 15, 2005).
Some genes that contribute to alcoholism have also been pinpointed, John Nurnberger Jr., M.D., Ph.D., of Indiana University's Institute of Psychiatric Research added (Psychiatric News, April 6). One of the more interesting, he indicated, is a gene on chromosome 4 that codes for the GABRA2 receptor. This gene is also a risk factor for drug dependence, he said.
Genes on chromosomes 9 and 10 seem to be implicated in nicotine dependence, Jonathan Pollack, Ph.D., chief of the Genetics and Molecular Neurology Research Branch at the National Institute on Drug Abuse, pointed out. Furthermore, these findings have been replicated by a number of scientific groups.
According to Cathy Barr, Ph.D., a professor of psychiatry at the University of Toronto, a number of genes that may contribute to attention-deficit/hyperactivity disorder (ADHD) have been found. Some of them look especially auspicious—for example, the genes for the dopamine receptor D4 and the dopamine transporter. Actually ADHD genes have been easier to find than geneticists expected, probably because ADHD is highly heritable, she said. Nonetheless, “each gene identified so far contributes only a small risk to the development of the disorder,” she conceded.
Sklar and colleagues screened some 500,000 snips of DNA from 1,461 individuals with bipolar disorder and from 2,008 controls to try to locate bipolar genes. This was the largest single whole genome study of bipolar disorder to date, she reported. Their biggest “hit”—the gene that seemed most likely to contribute to the illness—was a gene on chromosome 12 that is involved in the passage of calcium through the cell membrane. In fact, calcium-channel blockers have been used with some success in treating bipolar disorder, so she and her colleagues are“ excited” about the finding, she said.
It looks as if rare genetic errors underlie certain cases of autism, Catalina Betancur, M.D., Ph.D., of the National Institute of Health and Medical Research at the University of Paris in France reported. For instance, she and her colleagues found a gene deletion on chromosome 22 in two brothers with autism and severe mental retardation, suggesting that the gene may have contributed to both conditions.
Some more common gene variants may also contribute to autism, Buxbaum noted. “Certain candidate genes have been studied in multiple labs and are beginning to be accepted by some researchers. . . . However, no common variant is accepted. I think that is where we are today.”
More Advances on Horizon
And in the rush to identify psychiatric genes, there are glimmerings of progress to come.
Christopher Ross, M.D., Ph.D., and colleagues put a gene called DISC 1 into transgenic mice, and it caused ventricular enlargement—one of the features of schizophrenia. This is the first transgenic mouse model for schizophrenia.
Credit: Joan Arehart-Treichel
It is now possible to incorporate genes suspected of causing schizophrenia into mice embryos and then follow the mice's development to evaluate the impact of those genes, Christopher Ross, M.D., Ph.D., a professor of psychiatry, neurology, and neuroscience at Johns Hopkins University, pointed out. Some of those genes will probably turn out to be active in neurodevelopment, others in nerve transmission, he predicted (Psychiatric News, October 5).
Some geneticists are now combining two innovative techniques—genome-wide association studies and neuroimaging—in a quest to unmask psychiatric genes. One of them is Steven Potkin, M.D., of the University of California at Irvine. For instance, he and his colleagues are imaging the brains of schizophrenia subjects and controls, noting differences between the two groups, and then looking for gene variants in the former that might explain those differences. “This is just a beginning; this is new territory,” Potkin said.
Indeed, as Francis Collins, M.D., Ph.D., director of the Human Genome Project, reported at the congress, some 60 genes that contribute to medical illnesses have been identified. He predicted that before long, more genes underlying psychiatric illnesses will have been found as well. For example, he said, geneticists trying to identify genes that contribute to bipolar disorder are at the point where geneticists attempting to identify genes that contribute to diabetes were somewhat earlier—they have ferreted out suspect gene areas and now need to zero in on the specific genes involved.
“I think you will find the next several years dramatic and exciting,” Collins declared. ▪



