Eating-Disorder Data Show Extensive Comorbidities
Binge eating disorder (BED) is the most common type of eating disorder in the United States and appears to be far more prevalent than other eating disorders such as anorexia and bulimia, according to the results of a large national survey.
According to the findings, 3.5 percent of women and 2 percent of men reported experiencing symptoms of BED currently or at some point during their lives. In contrast, 0.9 percent of women and 0.3 percent of men reported symptoms of anorexia, and 1.5 percent of women and 0.5 of men reported symptoms of bulimia.
The results appeared in the February 1 Biological Psychiatry.
“Previously, we didn't know the extent of the prevalence of binge eating disorders,” first author James Hudson, M.D., Sc.D., told Psychiatric News. “We were surprised that it was more common than both anorexia and bulimia combined.”
Hudson is director of the psychiatric epidemiology research program at McLean Hospital and a professor of psychiatry at Harvard Medical School.
The findings are based on data collected through the National Comorbidity Survey Replication, a nationally representative sample of the U.S. population. The household survey was conducted among more than 9,282 English-speaking adults over age 18 on a face-to-face basis between February 2001 and December 2003.
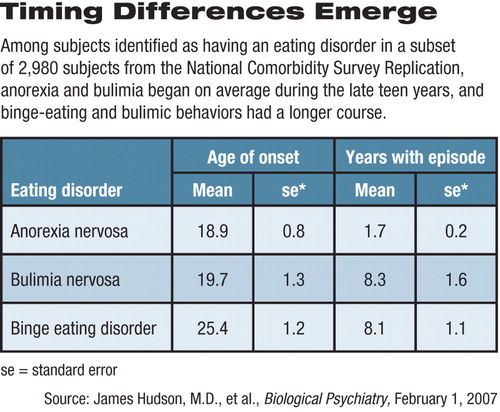
Hudson and his colleagues completed an analysis on a randomly chosen subsample consisting of 2,980 subjects and determined whether they had ever experienced an eating disorder based on questions from the World Health Organization Composite International Diagnostic Interview (CIDI).
Researchers used questions from the diagnostic interview to assign diagnoses of anorexia nervosa, bulimia nervosa, or BED to subjects based on DSM-IV criteria. Currently, the criteria for BED are listed in Appendix B of the DSM-IV-TR under the heading “Criteria Sets and Axes Provided for Further Study.” The syndromes or conditions are listed in this section pending further research that could provide scientific evidence warranting the conditions' status as a formal disorder.
The only instance in which the survey diverged from DSM criteria was for duration of symptoms classified under binge eating disorder—the DSM-IV requires a minimum of six months of regular eating binges, whereas the CIDI requires a minimum of three months of symptoms.
Hudson and his colleagues found that 2.8 percent men and women in the sample reported current or past symptoms of BED, and smaller proportions reported current or past symptoms of bulimia (1 percent) and anorexia (0.6 percent).
Many Subjects Sought Help
The mean number of years that subjects experienced symptoms of bulimia and BED (8.3 and 8.1, respectively) was significantly higher than that of anorexia (1.7 years).
Findings from prior studies often involved patients who had been hospitalized or had severe forms of the disorder. Thus, said Hudson, “We had long thought that anorexia was a persistent and chronic condition. These findings suggest that there are people in the community who have it for shorter periods of time, so it need not be a chronic and devastating illness.”
He also emphasized, however, that anorexia can be a “serious, devastating, and fatal condition.” By studying the factors associated with a short duration of illness, he said, researchers may be able to learn how to prevent more severe cases.
In addition, Hudson found that more than half (56.2 percent) of respondents with anorexia, 94.5 percent of those with bulimia, and 78.9 percent of those with BED met criteria for at least one other DSM-IV disorder, including mood and anxiety disorders, impulse-control disorders, and substance use disorders.
Half of those with anorexia (50 percent) and BED (51.2 percent) reported receiving treatment for emotional problems at some time in their lives, according to the findings. Slightly more than 63 percent with bulimia sought help for an emotional problem at some point during their lives.
The majority of those with an eating disorder sought help in the general medical sector.
Hudson also noted that those with BED were about five times more likely than those without it to have a body mass index of 40 or higher.
BED Linked to Obesity Epidemic
Due to the relatively high prevalence of BED in comparison with other eating disorders, the duration of the illness, and its association with obesity, Hudson considers BED a major public health problem and one of the factors underlying the obesity epidemic in the United States. He also said it warrants inclusion in DSM-V, which is scheduled for release in 2012.
According to William Narrow, M.D., M.P.H., associate director of APA's Division of Research, the DSM-V Eating Disorders Workgroup is reviewing the literature on BED to determine whether it should be categorized as a mental disorder in the DSM-V.
Hudson said that primary care doctors and other clinicians should become aware of the symptoms for binge eating (see Original article: box) to improve recognition and treatment of BED. The symptoms of BED have the potential to be reversed through cognitive-behavioral techniques or through use of certain medications, he noted. Intervention could make a significant impact in the obesity epidemic, he added.
The NCS-R is funded by the National Institute of Mental Health, National Institute on Drug Abuse, Substance Abuse and Mental Health Services Administration, Robert Wood Johnson Foundation, Eli Lilly and Co., and John W. Alden Trust.
An abstract of “The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication” is posted at<www.journals.elsevierhealth.com/periodicals/bps/article/PIIS0006322306004744/abstract>.▪



