Opioid Prescribing May Be Increasing
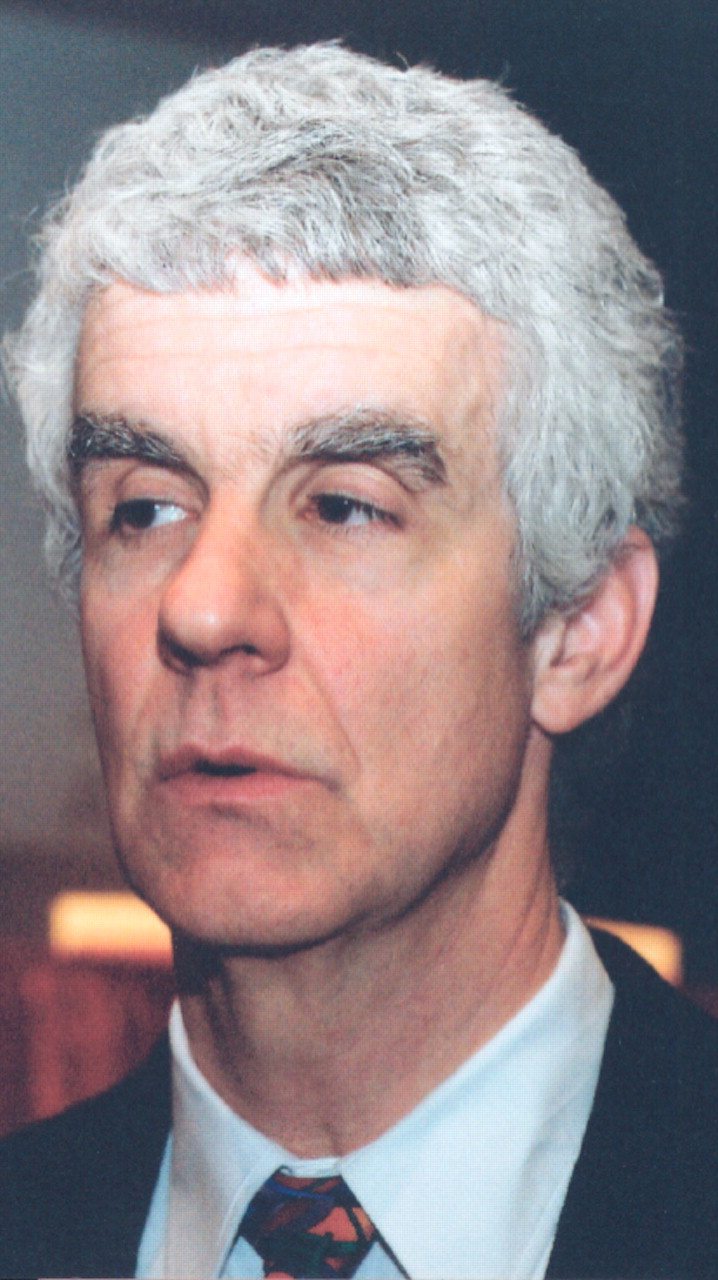
Mark Sullivan, M.D.: “A diagnosis of depression while receiving opioid therapy predicted opioid dependence even when possibly confounding factors were taken into consideration.”
Credit: Joan Arehart-Treichel
Many of the Americans who use opioid analgesics today are cancer patients, Kathleen Foley, M.D., an attending neurologist at Memorial Sloan-Kettering Cancer Center, reported at a recent conference on pain, opioids, and addiction (see “Search Is On to Discover 'Perfect' Pain Killer”). One-third of cancer patients in active therapy and two-thirds of patients with advanced cancer receive opioid analgesics for their pain, she said.
During the 1940s and 1950s physicians were reluctant to give opioid analgesics to cancer patients for fear that the patients would become addicted to them, she pointed out. But by the 1980s physicians had become more open to the idea of using the medications. Also, the Medicare hospice benefit was created, which rapidly spread the use of opioid treatment for cancer and other terminally ill patients whose lives were in their final months. The availability of opioid treatment for cancer patients has increased still more since then, she pointed out. For example, new methods of opioid drug delivery have revolutionized pain management in cancer patients. Also, terminal cancer patients have access to some 4,000 hospices and to some 2,000 hospice physicians who have been trained in the delivery of opioids and other pain-relieving medications.
As far as Americans who use opioid analgesics for noncancer pain, they often have back pain or arthritis, and they tend to be Caucasian more often than black or Hispanic, reported Mark Sullivan, M.D., Ph.D., a professor of psychiatry at the University of Washington, at the conference.
Sullivan also maintains, on the basis of two studies he and his colleagues conducted, that the prescribing of opioid analgesics in the United States is increasing. In one of these investigations, they evaluated opioid prescribing in the Group Health Cooperative, a Seattle HMO, from 1997 to 2005. They found a 150 percent increase in the prescribing of low-dose opioids for chronic use and also an increase, although smaller, in the prescribing of high-dose opioids for chronic use.
Moreover, opioids are being prescribed for longer periods than they used to be, Walter Stewart, Ph.D., pointed out. He is director of the Geisinger Center for Health Research in Danville, Pa.



